What Does 2016 Have In Store For You?
Therapists can heave a sigh of relief as the dreaded annual cuts are no longer on the horizon. However, therapy caps are still in place and the expected impact on reimbursement due to revised relative value units (RVUs) will be zero in 2016.
The Centers for Medicare and Medicaid Services (CMS) released the first proposed physician fee schedule since the repeal of the sustainable growth formula. The proposals included 2016 payment rates for Medicare-billed services, updated quality provisions, and revisions to payment policies, outlined in the proposed rule published in the July 7 Federal Register.
Proposed Payment Rates
The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) called for a 0.5 percent increase and budget neutrality adjustment of 0.9999, which has been reflected in the proposed 2016 conversion factor of $36,1096. However, the work values, practice expense values, and malpractice expense values related to physical therapy services remain the same. The mix of services provided by individual physical therapy practices will determine what will be the actual impact on their payment rates, points out the American Physical Therapy Association’s (APTA’s) July 10 news release.
Changes in Relative Value Unit (RVU) Impacts
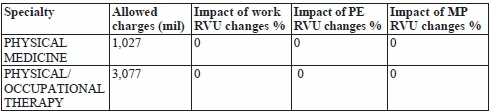
“The payment impacts in this proposed rule reflect averages by specialty based on Medicare utilization,” CMS said in the proposed rule.
Table 45 — CY 2016 PFS Proposed Rule Estimated Impact on Total Allowed Charges by Specialty
Source: CMS 2015 MPFS at www.federalregister.gov/articles/2015/07/15/2015-16875/medicare-program-revisions-to-payment-policies-under-the-physician-fee-schedule-and-other-revisions#h-8.
Review On The Horizon
Therapists commonly report ten CPT® codes, including 97032 (electrical stimulation), 97035 (ultrasound therapy), 97110 (therapeutic exercises), 97112 (neuromuscular reeducation), 97113 (aquatic therapy), 97116 (gait training), 97140 (manual therapy), 97530 (therapeutic activities), 97535 (self-care management training), and G0283 (electrical stimulation other than wound). CMS identified these among the 118 total “high expenditure” codes with Medicare allowed charges of $10 million or more. These codes, which have not been re-valued or reviewed since 2009 or earlier, have been identified for review by CMS because there may have been changes in direct practice inputs and how providers work in relation to these services.
CMS intends to “compare the total RVUs of the relevant set of codes (by volume) in the current year to the update year, and divide that by the total RVUs for all codes (by volume) for the current year” to arrive at the appropriate adjustment.
Don’t Risk This Payment Reduction
In keeping with the provisions of the Affordable Care Act, PQRS measures that PTs need to report will be more or less the same as in 2015. The twist in the tale is that those therapists who don’t participate successfully in PQRS reporting in 2016 risk taking a 2.0 percent hit in payment in 2018. You will also need to make all PQRS measures available for public reporting annually, although PTs will not be part of the value-based modifier program in 2016. These measures include:
Exception: However, if you render services in tandem with any home health agency that is situated in a state where the pilot Medicare’s Value-Based Purchasing (VBP) program for home health agencies is being run, you’ll have to worry about your outcomes affecting your reimbursement sooner rather than later. Nine states, namely, Massachusetts, Maryland, North Carolina, Florida, Washington, Arizona, Iowa, Nebraska, and Tennessee, have been named in the proposed pilot VBP. These states were chosen based on characteristics such as agency size, utilization, and patient population characteristics.
CMS is not allowing any PQRS exemptions on the basis of low volume or hardship. “All EPs (eligible providers) who furnish covered professional services must participate in the PQRS each year by meeting the criteria for satisfactory reporting — or, in lieu of satisfactory reporting, satisfactory participation in a QCDR — to avoid the PQRS payment adjustments,” CMS said in the proposed rule.
The reasoning behind the insistence on participation in PQRS or, at least QCDR, is to emphasize “the importance of collecting patient-reported data and the ability to impact care at the individual patient level,” and ensure greater patient satisfaction, points out the Federal Register article.
Modifications To Stark Law
CMS has proposed certain major provisions related to the Stark Law “to accommodate delivery and payment system reform, to reduce burden, and to facilitate compliance,” and “to expand access to needed health care services.” While the idea behind the law is to prevent conflicts of interest, CMS recognizes that the three-part aim of “improving the experience of care, improving the health of populations, and reducing per capita costs of health care,” could impose further burdens on providers.
Primary among these are definition of remuneration; writing requirement; term requirement; and “takes into account.” “Many compensation exceptions to the Stark Law prohibit compensation that ‘takes into account’ referrals,” says Hall Render in a July 9 Health Law blog. “The Proposed Rule, if implemented as currently proposed, would update the Stark Law regulations to account for recent changes relating to health care reform and advancements in patient care and payment methodologies,” it added.
Remember, physical therapy services, occupational therapy and speech-language pathology services fall under the category of Designated Health Services (DHS) encompassed within the Stark Law.
Resources: You have until Sept. 8 to comment on any of the proposals listed above. For more details on the proposals, check https://s3.amazonaws.com/public-inspection.federalregister.gov/2015-16875.pdf or www.federalregister.gov/articles/2015/07/15/2015-16875/medicare-program-revisions-to-payment-policies-under-the-physician-fee-schedule-and-other-revisions#h-8.
To see the complete APTA news release, visit www.apta.org/PTinMotion/NewsNow/?blogmonth=7&blogday=10&blogyear=2015&blogid=10737418615. For more on the proposed Stark Law modifications, see blogs.hallrender.com/blog/cms-issues-sweeping-proposed-rule-with-many-stark-law-modifications.