Document Measurable Objective And Interventions For Restorative Care
Formal therapy needs might arise out of long term stays.
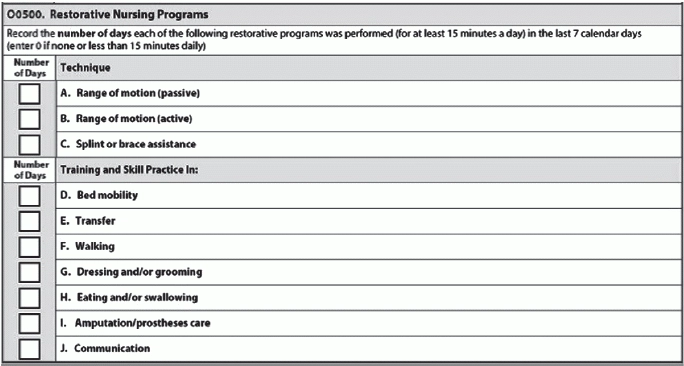
Don’t let the specific criteria you’ll need to code O0500 trip you up.
Take charge by coding the Restorative Nursing Programs section of the MDS correctly with this advice.
Show Program Implementation
“CMS considers this a program, so documentation of the implementation of a program needs to be in place,” says Patricia Boyer, MSM, RN, NHA, president of Boyer & Associates, LLP in Brookfield, WI. “In other words, minutes of care and documentation of what care was provided needs to be in place.”
Usually, you’ll find documentation of the program after a resident is discharged from formalized physical, occupational, or speech therapy. But sometimes, you’ll find documentation after admission, if the resident begins a restorative nursing program when he’s admitted with restorative needs but isn’t a candidate for formal rehab therapy. In other instances, the resident may have restorative needs that arise during a longer-term stay or in conjunction with formalized therapy.
Beware: Although you cannot take credit for the time the physical therapist spent on treatment, residents can be on skilled therapy and restorative nursing at the same time — but the interventions and goals cannot be the same.
Check for Specific Staff Training
“Staff providing the restorative care must be trained in that component of care,” Boyer instructs. “Anyone can provide restorative care as long as they have been trained.”
Remember: In addition to proper training, a registered nurse or licensed practical nurse must supervise the restorative nursing program’s activities. You don’t need a physician’s order for restorative nursing, but you do need the licensed nurse supervision.
Don’t Just Say ‘Restorative Care’
Crucial: “Each program must be reflected in an individualized plan of care with measurable goals and specific interventions (it can’t just say restorative care),” Boyer points out.
You must have a measurable objective and interventions documented in the care plan and medical record. If the care team is revising the care plan, document in the resident’s medical record the appropriate reassessment of progress, goals, and duration/frequency for the restorative nursing program.
Code Only What the Resident Actually Received
Additionally, pay attention to the dates on the patient’s record when you’re coding for restorative nursing services. “You should only code on the MDS what the resident actually received, not what was scheduled,” Boyer cautions.