Get the Deserved Reimbursement by Selecting Appropriate E/M Guidelines
While deciding whether you need to go with the 1995 or 1997 E/M guidelines, you’ll need to check on how your practitioner documents, what details are captured by your clinician, and the key components of the physical examination to help you make your decision.
Focus on the 1995 vs. 1997 Differences
There are two sets of documentation guidelines you should be familiar with before trying to determine the level of the physical examination key component for your E/M coding: 1995 and 1997 guidelines.
Both sets of guidelines help you determine which of the following four levels of examinations your provider completed during an E/M service: problem-focused, expanded problem focused, detailed, and comprehensive. The level of exam is a factor in determining which code you can report: 99201-99205 (Office or other outpatient visit for the evaluation and management of a new patient, which requires these 3 key components ...) for new patients or 99212-99215 (Office or other outpatient visit for the evaluation and management of an established patient, which requires at least 2 of these 3 key components ...) for established patients.
The exam element is the most significant difference between the two sets of guidelines.
1997: The 1997 guidelines include specific physical exam elements that must be addressed in the documentation, both for a general multi-system exam and for single organ system examinations. If a physician addresses elements other than those specified in the guidelines, the physician will not necessarily receive credit for those elements in the level of service. Also, if the language pertaining to an exam element included in the documentation differs from the language included in the guidelines, an auditor who has not had much clinical experience may inadvertently exclude the element from being credited in the level of service.
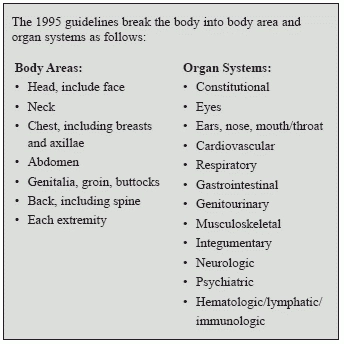
1995: The 1995 guidelines are much more general and, therefore, much less restrictive in a way. They allow the physician to make any comment in any of the designated body areas and/or organ systems he examines. What the physician examines within the areas and systems and the wording he or she chooses to document are ultimately decided by the physician. See the chart to see how to count the elements for each set of guidelines and choose your code level.
Choose the Best Guidelines Per Encounter
You don’t have to pick one set of guidelines and stick with them every time you code an E/M service. You can switch between 1995 and 1997 from one service to the next. “Given that per Medicare, ‘carriers and A/B Medicare Administrative Contractors are to continue reviews using both the 1995 and 1997 documentation guidelines (whichever is more advantageous to the physician)’, physician practices are not restricted to using only one of the guidelines,” says Marvel J. Hammer, RN, CPC, CHCO, president of MJH Consulting in Denver. You can choose whichever set of guidelines is most advantageous for each encounter, says Suzan Berman, MPM, CPC, CEMC, CEDC, manager of physician compliance auditing for West Penn Allegheny Health Systems, Pittsburgh, Penn. For more details, check this MAC website on http://www.cahabagba.com/part-b/education/evaluation-and-management-services-information-center/
Essential: The key, however, is that you have to use either 1995 or 1997 guidelines for a single encounter. Remember, the guidelines differ primarily in the reporting of the physical examination. The other two key components — history and medical decision making –are essentially the same, no matter which physical examination guidelines you use.
Caution: “Practices should be aware of any special requirements that are part of their contracts with their insurers,” warns Marcella Bucknam, CPC, CCS-P, CPC-H, CCS, CPC-P, CPC-I, CCC, COBGC, internal audit manager at CHAN Healthcare in Vancouver, Wash.
So which should you use? That depends on your provider and how he documents. “Typically, the 1995 documentation guidelines are going to be more advantageous for most practices,” Bucknam explains. “This is because they are more flexible and also because they reflect the way most physicians were taught to document. However, some physicians may have been taught or may have developed good documentation practices around the 1997 guidelines, and this may be advantageous to them.”
Bottom line: Choosing between the two guidelines can be difficult, but until a better system is in place, coders should use the set that is most beneficial for each visit note. “Some specialties will benefit from the use of 1995 rules; others will benefit from the use of the 1997, so make sure to look closely when making these changes in your practice,” says Becky Boone, CPC, CUC, with The Coding Network and the University of Missouri Internal Medicine Department in Columbia.
Be Careful with Exam Templates
Having your provider use a paper template or one within your EMR can be helpful to ensure he captures every piece of his exam, but use caution. “Templates are a good way to ensure capturing of all elements of the exam, but physician training can help with this also,” Boone says. “If you do use a template, it really is a good idea to tailor it to the specialty.”
“Templates can be useful as long as they are not abused,” Bucknam agrees. “The appropriate exam is the exam that the physician thought was needed in order to appropriately assess the patient’s presenting problem. Putting in a bunch of other useless stuff is inappropriate and may raise questions about medical necessity.”
Warning: Medical necessity must guide the exam -- basically, your provider may not need to examine every system trying to reach a higher E/M level. “The physician should document everything he needed to check in order to appropriately assess the patient’s condition but should not do ‘extra’ exam elements simply to meet a level of service,” Bucknam says.