Visualize E/M Coding Bliss Next Year with 3 Facts
Hint: You’ll want to clock your time more accurately next year. You’ve got less than a year to prepare for the upcoming updates to the E/M codes, but with a bit of preparation, you’ll be coding these services like an ace from day one. Check out the following three facts about the way you’ll report these services in the new year. 1. Know the Time Guidelines Medical practices are well aware of the fact that in 2021, you’ll select new and established outpatient E/M codes based on the level of medical decision making (MDM) your provider uses/documents during the encounter or based on the total time of the encounter. But one reader wrote and asked whether the time parameters will be the same in 2021 as they are today. The answer is no. Effective Jan. 1, CPT® will replace the words “typical time” with the words “total time spent on the day of the encounter.” Check out this chart that outlines the current typical times as well as the times you’ll see in 2021: Example: Suppose a pulmonologist meets a new asthmatic patient in the office who is presenting with wheezing for more than two months, and the visit consists of moderate medical decision making and lasts 45 minutes. If that’s the case, you’ll report 99204 (Office or other outpatient visit for the evaluation and management of a new patient…) “You do not need both MDM and time,” says Raemarie Jimenez, CPC, CIC, CPB, CPMA, CPPM, CPC-I, CCS, senior vice president of product at AAPC and coding liaison to the AMA CPT® Editorial Panel. In other words, you could look at either the time in this example (45 minutes) or the level of MDM (moderate level), and this will direct you to 99204. Note: The time in 2021 will also include any time spent outside of the face-to-face encounter on the calendar day in activities directly related to patient management and the encounter (as outlined in the link above). You’ll note that the highest new patient E/M code (99205) time threshold only goes up to 74 minutes, but if you exceed that time, you’ll be able to report a prolonged services add-on code that is temporarily referred to as +99XXX. “You can report 99205 with the prolonged services code when 75 minutes is reached,” Jimenez says. 2. Confirm the Necessary Documentation Another reader wrote to Pulmonology Coding Alert asking whether the documentation requirements will change effective January 1. Although the government isn’t mandating specific documentation changes, you will have to ensure your providers include enough in their documentation to allow you to select codes under the new parameters. When you are billing on time, your documentation should note exactly how much time was spent on each aspect of the visit, and what you did during those periods, “although thus far no such explicit instruction is in CPT® nor has it come down from CMS,” advises Glenn D. Littenberg, MD, MACP, FASGE, AGAF, a physician and former CPT® Editorial Panel member in Pasadena, California. “At minimum, the total time spent on the day of encounter should be recorded, and an auditor should be able to review the note and see that the complexity of the problems dealt with would ‘logically’ entail that much time on the encounter date,” he adds. Remember that your documentation should be thorough whether you’re billing based on MDM or on time. “A doctor should document correctly regardless of the E/M coding and billing implications,” says Henry Borkowski MD, CEO of OmniMD. “If you’re documenting the right way now, it will make code selection easier down the line.” 3. Consult New Table of Elements Anyone who calculates MDM is familiar with the table of risk, which allows coders to select the appropriate MDM level, says Deena Wojtkowski, CPC, CEMC, CCP, vice president of client services with ebix, Inc. But several readers have wondered whether that table of risk will remain the same next year. The short answer is no. To replace it, you’ll find a table of elements, which includes several updated options. For instance, the existing “Number of diagnoses or management options” element has merged with CMS’s “Presenting problem(s)” to become “Number and complexity of problems addressed” in the new chart. The second element, labeled the “Amount and/or complexity of data to be reviewed and analyzed” has been completely redefined. Each level in this element has two to three categories, each comprised of various combinations of tests, documents, interpretations, and so on. So, too, has the third element, which will become “risk of complications and/or morbidity or mortality of patient management.” The American Medical Association (AMA) has also used this E/M overhaul to examine the terminology it has traditionally used to define the codes. Taking a mid-level code (such as 99203/99213) as an MDM example, that means clearing up confusion surrounding a concept like “morbidity,” which the AMA now defines as “a state of illness or functional impairment that is expected to be of substantial duration during which function is limited, quality of life is impaired, or there is organ damage that may not be transient despite treatment.” Similarly, the AMA has pinned down the term “independent historian,” which it defines as “an individual (e.g., parent, guardian, surrogate, spouse, witness) who provides a history in addition to a history provided by the patient who is unable to provide a complete or reliable history (e.g., due to developmental stage, dementia, or psychosis) or because a confirmatory history is judged to be necessary.” Hopefully, such definitions will make these 2021 revisions to office and outpatient E/M levels easy to implement when they take effect on Jan. 1 and better allow the coder/auditor to clearly educate physicians and apply the MDM guidelines to the auditing process. Resource: To review the new MDM table, visit https://www.ama-assn.org/system/files/2019-06/cpt-revised-mdm-grid.pdf.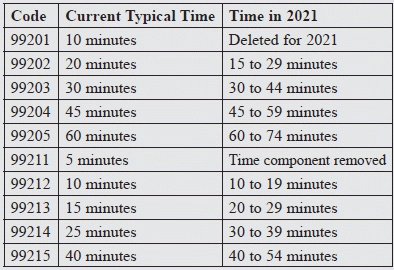
Source: The AMA’s CPT® E/M Office or Other Outpatient and Prolonged Services Code and Guideline Changes, available at https://www.ama-assn.org/system/files/2019-06/cpt-office-prolonged-svs-code-changes.pdf.

