Discover the Truth About PFT Component Code Misconceptions
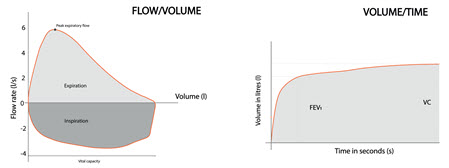
Hint: You can report 94150 and 94200 separately. As a pulmonology coder, you think you can call out common pulmonary function test (PFT) codes without a second thought. But can you really? There are a lot of commonly held myths about individual PFT service codes that can affect accurate PFT coding. So to help you, we’ve debunked three of the most widely held PFT service coding myths. Myth 1: You can report 94150 with spirometry on the same claim. You don’t have to look too much farther than the parenthetical note following 94150 (Vital capacity, total (separate procedure)) to debunk this myth. The parenthetical note after 94150 instructs you to not report the code in conjunction with spirometry codes, such as 94010 (Spirometry, including graphic record, total and timed vital capacity, expiratory flow rate measurement(s), with or without maximal voluntary ventilation) and 94060 (Bronchodilation responsiveness, spirometry as in 94010, pre- and post-bronchodilator administration). Total vital capacity is already included in spirometry procedure codes, such as 94010 and 94060. Code 94150 is designated as a separate procedure, so you can’t report it along with more extensive respiratory testing because you would be billing double for the vital capacity test. According to the Separate Procedures section of the CPT® guidelines, “The codes designated as ‘separate procedure’ should not be reported in addition to the code for the total procedure or service of which it is considered an integral component.” “Basically, 94150 is included as part of 94010, as well as 94060, so unless there is an extenuating circumstance that would allow modifier 59 (Distinct procedural service) to be appended, these cannot be coded together,” says Julie Davis, CPC, CRC, COC, CPMA, CPCO, CDEO, AAPC-Approved Instructor, risk adjustment manager of Physician Health Partners in Parker, Colorado. The 2023 Medicare Physician Fee Schedule (PFS) assigned a “B” status to 94150, which means the code is not paid separately. At the same time, to prevent unbundling, the National Correct Coding Initiative (NCCI) implemented code-pair edits for the code. NCCI also established a medically unlikely edit (MUE) of “0” for professional claims. Therefore, NCCI discourages 94150 from being inappropriately billed, and prevents 94150 from being inappropriately reimbursed. Myth 2: A diffusing capacity code requires a modifier to report it with 94375. This myth is incorrect simply because +94729 (Diffusing capacity (eg, carbon monoxide, membrane) (List separately in addition to code for primary procedure)) is an add-on code. You don’t need modifiers to assign add-on codes correctly. Instead, you just need to report an appropriate primary procedure code. The debunked myth implies diffusing capacity can be reported with 94375 (Respiratory flow volume loop), which is true. You’d assign 94375 as the primary procedure code and follow it up with +94729. “There aren’t any coding conflicts with these two codes,” Davis adds in reference to the NCCI procedure-to-procedure (PTP) edits. You can report flow volume loop testing and diffusing capacity services individually if your provider performs these services separately from a PFT, and your code selection will be easier with an understanding of what the procedures entail. Flow volume loop testing: During flow volume loop testing, the provider examines a complete respiratory cycle and graphs the airflow rate as a function of the patient’s lung volume. The complete respiratory cycle consists of forced inhalation followed by forced exhalation. This test is typically performed without bronchodilator administration, and the results are plotted on a curve, which looks like a loop, to evaluate the patient’s pulmonary function. A provider uses a flow volume loop test to determine if the airflow is appropriate for the lung’s volume. A provider will also perform a flow volume loop test to evaluate the patient’s breathing patterns to determine if there is an obstruction in the upper or lower airways. You may notice the terms “flow volume loop” or “FVL” in the provider’s documentation. Diffusing capacity testing: In a diffusing capacity study, the pulmonologist examines the patient’s lungs’ ability to transfer gases into and out of the bloodstream. As the patient inhales, oxygen is absorbed into the blood and when the patient exhales, carbon dioxide moves from the blood into the lungs and out of the body. Also, you may report add-on code +94729 with 94010, according to the parenthetical note listed under +94729. Caution: Be sure that the physician reports 94010 if the test meets criteria for billing spirometry instead of flow volume loop. Physicians may be tempted to report the higher paying service (94375), when the more comprehensive test is performed (94010). Myth 3: You can never report 94200 with a PFT. This myth is a tricky one to debunk but knowing when the provider performed the breathing capacity testing will ease your confusion. Yes, breathing capacity (94200 [Maximum breathing capacity, maximal voluntary ventilation]) is inherently included in PFTs, such as spirometry and oscillometry. But there are instances when a pulmonologist may perform the individual procedure separately. One reason is that “the documentation supports a different session (meaning the patient was seen, left, and was called back to do the other testing),” Davis says. Scenario: A patient presents to the pulmonologist for spirometry without bronchodilator administration. The patient leaves the office once the test is completed. While reviewing the results, the pulmonologist notices an abnormality and requests the patient returns that day for another breathing capacity test. In this scenario, you’ll report 94010 for the initial spirometry exam. You’ll then report 94200 with 59 or one of the X{EPSU} modifiers depending on the payer. Check with the individual payer preferences to see which modifier they’d prefer to specify that the breathing capacity code is separate from the initial spirometry. Another reason where you could report 94200 with a PFT code is “if the services were provided by two different providers on the same day, then each could bill for what they performed,” Davis says. Let’s re-examine the same scenario above, only with a different pulmonologist performed the separate 94200. In that case, you’d append 94200 with XP (Separate practitioner, a service that is distinct because it was performed by a different practitioner). Of course, you should double-check your payer preferences in case they require a different modifier.