Master Cystourethroscopy Coding With These Case Studies
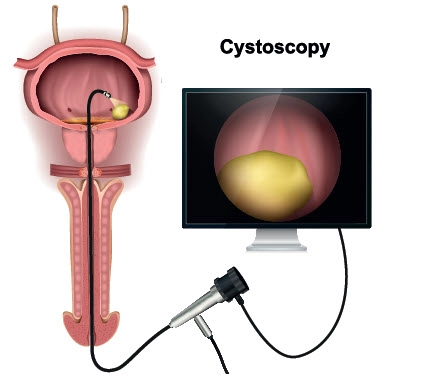
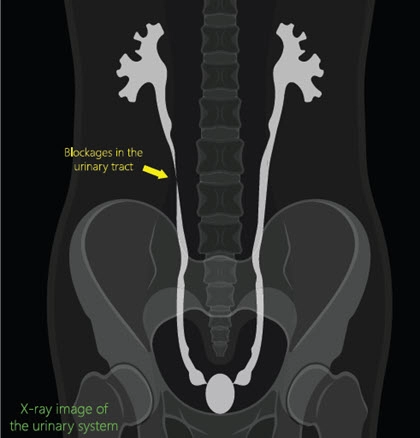
Maneuver between guidelines and expert advice to drive the point home. A surgical specialty like urology requires some serious attention to detail in order to dissect an operative report into its most fundamental components. Most coders can attest to the dangerous ease with which you can get lost in the translation process of converting a surgeon’s operative report into one or more CPT® codes. That’s why we’re here to help you avoid this dilemma by breaking down one of the more common urological surgeries — cystourethroscopies. As you’ll see, it takes a trained eye to differentiate between each type of cystourethroscopy code. Use these sample operative reports to kick-start you on your way to cystourethroscopic coding success. Consider Codes From 52000 Through 52010 Using some real-world clinical examples, we’ll look at portions of an operative report from a few different kinds of cystourethroscopic procedures. For the purposes of this article, you’ll be working with some of the following cystourethroscopy codes listed under the 52000-52010 range: Don’t Reach for Code 52001 Without Supportive Documentation Op report #1: The patient was brought to the operating room, placed in lithotomy position. His lower abdomen and genitals were prepped and draped in sterile fashion. I introduced the rigid cystoscopy though the urethral meatus. Within the bladder there was much debris, and the prostatic urethra was normal. At this point, a catheter could not be passed into the bladder. Therefore, I made an incision in the suprapubic area using a surgical blade, and a 22-French catheter introducer was pushed through the incision into the bladder. I put a guidewire into the bladder and then a 20 French catheter was applied over the guidewire all the way into to the bladder. The bladder was irrigated free of its debris and is functioning adequately. You might find numerous reasons to consider this surgical report challenging due to the diagnostic and therapeutic components. Your initial step is to identify exactly what services the surgeon performed. First, the surgeon performed a diagnostic cystourethroscopy, documenting that the bladder and prostatic urethra were functioning properly. Due to unknown complications, the surgeon could not introduce a catheter into the bladder. The surgeon subsequently performed a punch cystostomy by incising the suprapubic area. Via this incision, the surgeon introduced a catheter into the bladder and then irrigated the bladder free of debris. As you can see in code range 52000-52010, there is no code that encompasses a cystourethroscopy with a bladder instillation. You might consider using 52001; however, the provider made no reference of obstructing clots. Even if the provider documented “debris” or similar verbiage, you should not consider code 52001. Instead, you should first report 51102 (Aspiration of bladder; with insertion of suprapubic catheter) for the punch cystostomy. In this clinical scenario, the cystourethroscopy is bundled into 51102 and is not separately billable. You should also code for the bladder irrigation by reporting code 51700 (Bladder irrigation, simple, lavage and/or instillation). You’ll find no bundling edit between codes 51102 and 51700, so no modifier is necessary. Use 52005 With or Without Extraneous Included Services Op report #2: A rigid cystoscope was placed into the urethra. Upon inspection of the bladder, both ureteral orifices have clear efflux. No evidence of bladder pathology. Bladder capacity was adequate. A #5-French cone tipped catheter was inserted into both ureteral orifices, respectively. Both ureters were normal. The upper collecting system was normal as well and the calices were sharp. Adequate drainage was noted bilaterally. The bladder was drained and inspected again. This operative report involves a cystourethroscopy with ureteral catheterization. Therefore, code 52005 is most appropriate. As noted in the code description, this code includes irrigation, instillation, and ureteropyelography, when performed. Billing note: For Medicare, you may report code 52005 for a unilateral or bilateral ureteral catheterization. For private and commercial carriers, add modifier 50 (Bilateral procedure) to 52005 for bilateral ureteral catheterizations. Don’t Consider 74420 Without Interpretation Op report #3: A 5-French end-hole catheter was placed in the right ureteral orifice. A right retrograde pyelogram under real-time fluoroscopy demonstrated no gross static filling defect or obstructive uropathy. Subsequently, a left retrograde pyelogram was performed. This demonstrated no gross static filling defect or obstructive uropathy. At this point, then the bladder was filled to capacity. The cystoscope was withdrawn. Here, you must consider the coding of both the cystourethroscopy and the retrograde pyelogram. “Most often, the surgeon will perform the retrograde pyelogram, but the radiological interpretation may be performed by a radiologist,” says Barry Rosenberg, MD, chief of radiology at United Memorial Medical Center in Batavia, New York. Assuming this is the case, you should not report 74420 (Urography, retrograde, with or without KUB) with 52005. The code description “exclusive of radiologic service” means that the surgical component of the pyelogram is included in 52005, but not the radiological interpretation. Therefore, the radiologist will bill out 74420 with modifier 26 (Professional component) for the interpretation. Coder’s note:” The urologist should report 74420-26 when performing both the pyelography and subsequently interpreting the results,” says Lindsay Della Vella, COC, medical coding auditor at Precision Healthcare Management in Media, Pennsylvania. “However, more often a separate radiologist will perform the interpretation and bill out 74420 with modifier 26,” Della Vella explains.