Sharpen Your Medicare Signature Knowledge
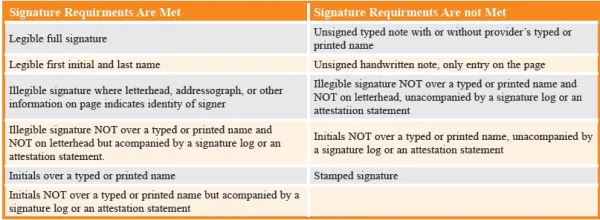
Resolving your questionable signatures prior to claim submission is key. In your urology practice, it’s likely that you encounter Medicare patients regularly, perhaps even daily or weekly. Therefore, mastering the skill of avoiding claim denials due to signature errors is crucial. Medicare mandates that any services provided or ordered must be verified by the author. This verification can be achieved through either a handwritten or electronic signature. Read on to learn the hard and fast rules of acceptable Medicare signatures. Rule 1: Medicare has guidelines that provider signatures must meet. Medicare requires that all services provided or ordered be authenticated by the author of the medical record. The appropriate method used for authenticating is either a handwritten or electronic signature. Take a look at some examples of medical records requiring a signature: Remember: Double-check signatures for dates. “All signatures must be dated,” and all “handwritten signatures must be hand dated,” Medicare Administrative Contractor (MAC) Palmetto GBA notes in guidance on its website (https://www.palmettogba.com). Rule 2: Medicare has a specific definition for an acceptable handwritten signature. Medicare defines a handwritten signature as “a mark or sign by an individual on a document to signify knowledge, approval, acceptance, or obligation.” If the provider’s signature is illegible, you may type or print the name below the signature. Rule 3: Medicare has strict rules on acceptable e-signatures for telehealth visits. Electronic signatures are valid — with some stipulations, indicates the Centers for Medicare & Medicaid Services (CMS). First, it’s critical to understand that you can’t just generate a signature with your electronic health record (EHR). Your practice’s software and computer systems must have protections against e-signature modifications; moreover, these standards should be stringent enough to correspond with any current signature laws on the books. Plus, “the individual’s name on the alternate signature method and the provider accept responsibility for the authenticity of attested information,” reminds the Medicare Learning Network (MLN) fact sheet “Complying with Medicare’s Signature Requirements,” which can be accessed at: https://www.cms.gov/outreach-and-education/medicare-learning-network-mln/mlnproducts/mln-publications-items/cms1246723. Additionally, Part B medications — “other than controlled substances” — should be ordered through an e-prescribing system, CMS guidance says. If you’re unsure of which types of e-signatures CMS accepts, take a look at a few of these examples: Tip: CMS encourages providers to check with attorneys and malpractice insurers to be sure their electronic signatures meet all the standards and regulations insurers have put forth. Rule 4: You are allowed to use a stamped physician signature under certain circumstances. Medicare will allow stamped signatures under very special circumstances, such as cases of authors with a physical disability, in accordance with the Rehabilitation Act of 1973. Under these circumstances, the author of the medical record who has the physical disability must prove their inability to sign the record due to their disability. By affixing the rubber stamp, the provider is certifying that they have reviewed the documentation. Rule 5: Illegible signatures must be submitted with additional documents for payment. In some cases, your provider’s signature may be illegible. If this happens, you can submit a signature log or an attestation statement with the claim. Signature logs and attestation statements support the identity of the illegible signature. You can automatically send the signature log/attestation statement along with your medical documentation to your MAC. Doing this will help avoid delays in the review process. Tip: You can submit an attestation statement if your provider’s signature is illegible. For Medicare to consider an attestation statement valid, the author of the medical record entry must sign and date the statement. The statement must also include the appropriate patient information. Caution: You can’t simply include a blank attestation statement with no patient identification information. The statement must be personalized for each patient and signed by the physician. Rule 6: Always keep a signature log. A signature log is a typed listing of the provider or providers identifying their name(s) with a corresponding handwritten signature(s). The provider’s credentials are required, and the signature log must be part of the patient’s medical record. Don’t miss: You may include the signature log on the same page where the initial or illegible signature is located or in a separate document. Just make sure that the signature log is a part of the patient’s medical record. A signature log can be created at any time and MACs will accept all submitted signature logs, regardless of the date they were created. Review this helpful chart to determine whether you’ve met the signature requirements dictated by CMS: