Review These Stent Placement Scenarios to Sharpen Your Skills
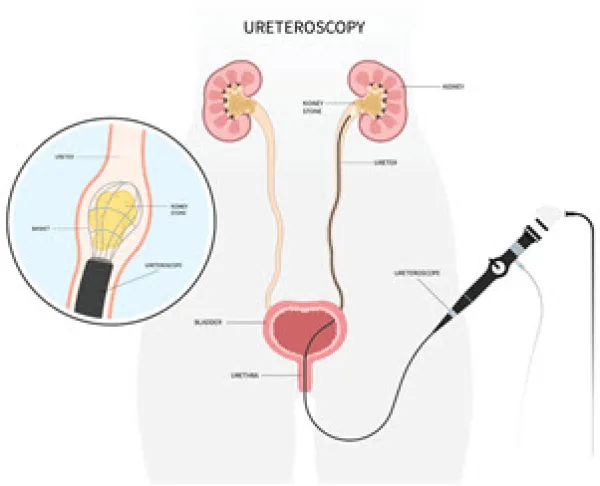
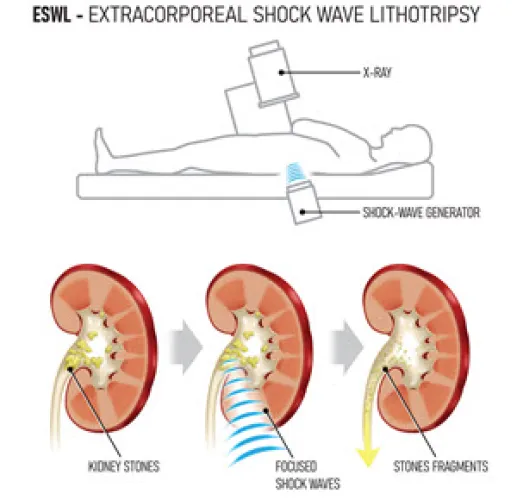
Don’t simply go with the flow when it comes to stents. Stent placement procedures are common in any urology practice. Regardless of your level of coding expertise, these stent placement scenarios offer useful insights and strategies to remember. Read on to learn more. Cystourethroscopy With Treatment of Stone(s) Scenario 1: The urologist performed a cystourethroscopy with lithotripsy including insertion of indwelling ureteral stent on the right ureter. Additionally, the physician documented “a 1.9 French basket was introduced through the ureteroscope, and the stone fragments were removed.” This is exactly as it is written in the dictated operative report. The urologist has submitted codes 52356 (Cystourethroscopy, with ureteroscopy and/or pyeloscopy; with lithotripsy including insertion of indwelling ureteral stent (eg, Gibbons or double-J type)) and 52352 (… with removal or manipulation of calculus (ureteral catheterization is included)) with modifier 59 (Distinct procedural service) appended. Is this correct? Answer: In this scenario, the provider performed the lithotripsy and stone removal at the same location in the right ureter; report only 52356 for this scenario. According to Stephanie Storck, CPC, CPMA, CUC, CCS-P, ACS-UR, longtime urology coding expert and consultant in Glen Burnie, Maryland, “The stone removal is part of the procedure if performed in the same location on the same side. If you break up the stone, it has to be removed. The documentation should support how the stone was removed after the lithotripsy was performed. There is no documentation to support the additional removal of the calculus except to state that it was done.” If the urologist performed the lithotripsy and stone removal at different locations, bill both codes (52356 and 52352) and attach modifier 59 or XS (Separate structure, a service that is distinct because it was performed on a separate organ/structure) to 52352. “The documentation should specifically support how the removal was a distinct service from the lithotripsy or the location of the removal,” says Storck. You may also differentiate the different sides by adding modifiers LT (Left side) and RT (Right side) to the appropriate CPT® code. CPT® states 52356 cannot be reported with 52332 (Cystourethroscopy, with insertion of indwelling ureteral stent (eg, Gibbons or double-J type) or 52353 (Cystourethroscopy, with ureteroscopy and/or pyeloscopy; with lithotripsy (ureteral catheterization is included) “when performed together on the same side.” Tip: The National Correct Coding Initiative (NCCI) edits reinforce that the stone removal work is part of the lithotripsy work by bundling 52352 with 52356. While there is a modifier indicator of “1” on this bundle — which means you can override the edit, if appropriate, using a modifier, such as modifier 59 or modifiers XE (Separate encounter, a service that is distinct because it occurred during a separate encounter), XS, XP (Separate practitioner, a service that is distinct because it was performed by a different practitioner), or XU (Unusual non-overlapping service, the use of a service that is distinct because it does not overlap usual components of the main service) — don’t report 52356 and 52352 together in this case. You should never use modifier 59 and other NCCI-associated modifiers to bypass an NCCI edit unless you meet the proper criteria for using the modifier. The documentation in the medical record must satisfy the criteria required by any NCCI-associated modifier that you use. Because your urologist performed both procedures in the right ureter, you can’t override the NCCI bundle. Stent Placement Prior to ESWL Scenario 2: The physician placed a stent prior to performing extracorporeal shock wave lithotripsy (ESWL). After the lithotripsy resulted in near resolution of the stone, they decided to remove the stent. This all took place during the same operative session. Are you able to bill 52332 or is there something else that could be billed for that work? Or is it best to just not bill the stent placement/removal at all? Answer: In this case, the stent was used for drainage during the procedure and was part of the procedure itself included in the surgical package/management of the complete procedure not for possible obstruction after the case. So, you should not bill separately for 52332. “If there were contralateral issues, or if the opposite kidney had confirmed stones, then a procedure performed on the side that did not have the ESWL could be reported. Somewhat frequently, patients with kidney stones have them on both the left and right side although the treatments might be different based on the patient’s severity. In theory, one side might be treated successfully with only a stent while the other side required both an ESWL and a completion stent placement,” says John Piaskowski, CPC-I, CPMA, CUC, CRC, CGSC, CGIC, CCC, CIRCC, CCVTC, COSC, specialty medicine auditor at Capital Health in Trenton, New Jersey, and AAPC consultant and committee chair. Ureteroscopy With Laser Lithotripsy and Tube Removal Scenario 3: The physician removed a nephrostomy tube and performed an antegrade ureteroscopy with holmium laser lithotripsy and removal of a ureteral stone, ureteral stent insertion through the nephrostomy, and nephrostomy tube exchange. The fragmented ureteral stone was basketed and removed. Finally, by using an antegrade approach, the physician placed a 4.8x26 JJ stent and a 20 French nephrostomy tube. Which codes should be reported on this claim? Answer: This procedure should be reported with code 50080 (Percutaneous nephrolithotomy or pyelolithotomy, lithotripsy, stone extraction, antegrade ureteroscopy, antegrade stent placement and nephrostomy tube placement, when performed, including imaging guidance; simple (eg, stone[s] up to 2 cm in single location of kidney or renal pelvis, nonbranching stones). Since the size of the stone was not indicated in the documentation, this is the appropriate code to use. If the documentation indicated a stone over 2 cm or stones in multiple locations, 50081 (...complex (eg, stone[s] > 2 cm, branching stones, stones in multiple locations, ureter stones, complicated anatomy)) could have been reported. “It is important to pay attention to the anatomical landmarks to identify the access and/or approach. In this case, the approach is antegrade because the provider begins in the kidney and goes with the urinary flow — antegrade — through the ureter. A retrograde flow would be an access through the urethra against the urinary flow to the ureter,” says Piaskowski.