Now on Codify by AAPC: Choose between QP and non-QP MPFS and anesthesia conversion factors in tools
The 2026 Medicare Physician Fee Schedule (MPFS) final rule introduced two separate conversion factors for codes on the MPFS as well as two separate conversion factors for anesthesia services. In each case, there is a higher conversion factor that applies for qualifying alternative payment model (APM) participants (QPs) under the Quality Payment Program (QPP) and lower conversion factor that applies for providers who are not QPs.
To ensure you have the correct amounts at your fingertips, Codify by AAPC by AAPC upgraded numerous tools you can choose between the QP and non-QP conversion factors. This includes fee schedule tools, fee schedule tabs on code details and code listing pages, Medicare National Correct Coding Initiative (NCCI) tools, Code Constructor, the CMS-1500 scrubber, anesthesia fee calculators, and more.
You can choose a default (QP or non-QP) to immediately see the calculation you need each time you open a tool. If you select a year prior to 2026, you will not have the option to choose QP or non-QP because prior years had only one conversion factor.
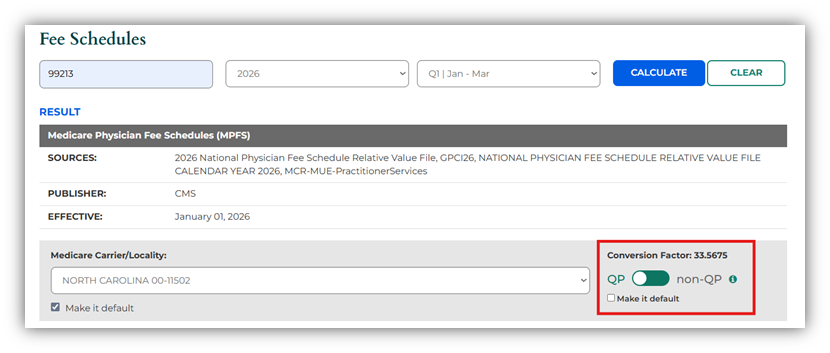
MPFS example: On the Fee Schedules page, select QP or non-QP after you enter the code, year, and quarter. The conversion factor is displayed above the toggle, and the option to make your selection the default is under the toggle.
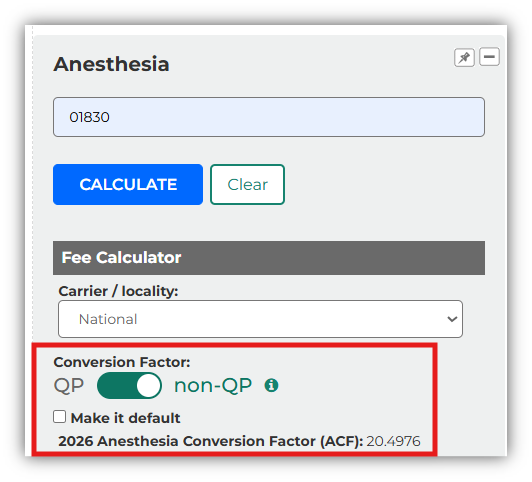
Anesthesia example: Subscribers to Codify by AAPC’s anesthesia add-on will see the anesthesia conversion factor options. For instance, in the Anesthesia widget, you can select QP or non-QP, choose which one to make default, and view the conversion factor based on your choices.
Note: Tools and data available may vary based on your Codify by AAPC package.