G codes hold the key to reporting quality measures in PQRS
Ready algorithms for you to zap through the G codes
CMS established G codes as part of HCPCS to report data when calculating quality measures – and they’re something every chiropractic group should be thinking of on a regular basis.
“Now is the time to start doing this. The nice thing about these codes is that it is helping to show Medicare that we as a chiropractic community have already addressed these issues with patients” says Doreen Boivin, CPC, CCA, with Chiro Practice, Inc., in Saco, Maine. “We just need to use the codes properly to document so that CMS recognizes the work the chiropractic community does. “
In the previous issue we discussed what PQRS is about. Now let’s get to know all you need about the quality measures and how to report the codes.
Chiropractors should be reporting on three quality measures:
Of these three measures, each has six to seven associated G codes that you report in conjunction with the appropriate CPT® procedure code, best describing the patient scenario. Read on for the lowdown on the requirements for two of these measures and how to select the appropriate G code in any situation.
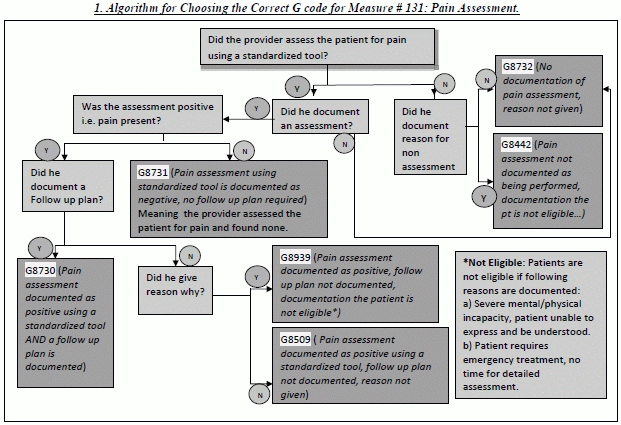
Quality Measure #131: Pain Assessment and Follow Up
The purpose of measure 131 is to collect data on pain assessment and the details of follow-up as treatment is carried out.
When gathering information from the patient, you need to use a standard assessment tool which is normalized and validated for the population. Examples include the Brief Pain Inventory (BPI), Faces Pain scale (FPS), McGill Pain Questionnaire (MPQ), and Multidimensional Pain Inventory (MPI) amongst many others. On each visit the provider must report:
a. Name of the assessment tool used.
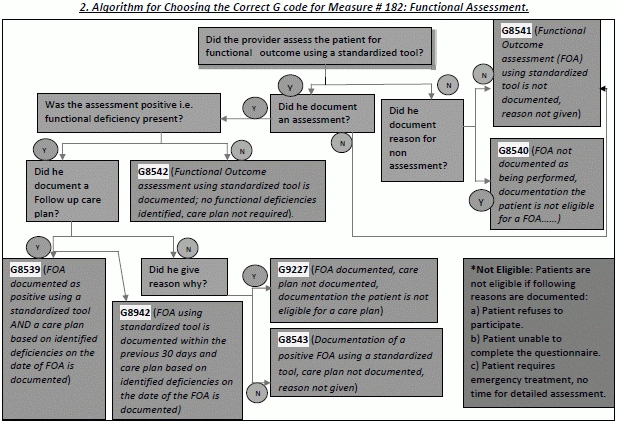
Quality Measure # 183: Functional Outcome Assessment
The purpose of this measure is to collect data on functional outcome assessment as it is carried out and the details of follow up as required.
Your provider should use a standard assessment tool which is normalized and validated for the population. Examples include Oswestry Disability Index (ODI), Roland Morris Disability Questionnaire (RMDQ), Neck Disability Index (NDI), etc.
On each visit the provider has to report:
a. Name of the assessment tool used for the purpose of functional evaluation. Merely naming the preceding measures’ pain assessment tool would not suffice, as some tend to think.
b. Whether he provided a standardized functional outcome assessment to the patient.
c. Whether he documented a care plan which enlists the goals, services, appointments etc. This tool is to be utilized a minimum of every 30 days as the one of the goals is to evaluate limitations every 30 days at least.
d. The appropriate G code. Possibilities include G8542 (Functional outcome assessment using a standardized tool is documented; no functional deficiencies identified, care plan not required), G8942 (Functional assessment using a standardized tool is documented within the previous 30 days and care plan, based on identified deficiencies on the date of the functional outcome assessment, is documented), and G8539 (Functional outcome assessment documented as positive using a standardized tool AND a care plan, based on identified deficiencies on the date of the functional outcome assessment is documented). Again remember to use these in conjunction with the CPT® codes 98940, 98941, and 98942.
Think About Future Implications
Tip: CMS strongly recommends that you report the G codes with a line item charge of one cent ($0.01). No, you won’t be getting this cent because MAC systems deny PQRS code lines for payment. However, the code is tracked in the National Claims History (NCH) for analysis so the penny amount allows the code to go through the system.
“By utilizing these codes you are indicating to Medicare your care for the patient is medically necessary. Implementing the use of the G codes is quite easy. It’s as simple as choosing a code based on your review and assessment. Why not use the documentation to show what you do and be reimbursed appropriately for the care given to the patient. “ comments Boivin.
The measures that CMS is tracking currently could be the forerunners of future criteria to prove necessity of care and receive adequate reimbursement. Knowing how the measures fit with your practice can benefit you now as you focus on delivering quality care, and help you prepare for additional quality focuses in the future.
Editor’s Note: In the next issue, learn about the third and the last measure of chiropractic quality reporting: Measure # 317, Preventive Care and Screening; the blood pressure screening and follow up.
b. Whether he provided a standardized pain assessment to the patient. (A clinical assessment tool may include characteristics of pain such as location, intensity, description, and onset/duration.)
c. Whether he provided a documented follow up plan to reassess the patient for pain, referrals, or notification of other care providers, or indicate continuation of the present treatment.
d. The appropriate G code. The two most common codes assigned with Measure #131 are G8730 (Pain assessment documented as positive using a standardized tool AND a follow up plan is documented), and G8731 (Pain assessment documented as negative using a standardized tool, no follow up plan required). Make sure you are submitting at least one of these three CPT® codes: 98940 (Chiropractic manipulative treatment(CMT);spinal, 1-2 regions), 98941 (Chiropractic manipulative treatment(CMT);spinal, 3-4 regions), 98942 (Chiropractic manipulative treatment(CMT);spinal, 5 regions)