Make the Grade With ACA's New PQRS Reporting Recommendations
Secure your 2017 payments by apt reporting of two measures.
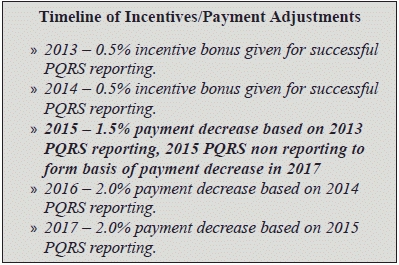
Though the deletion of measure 317 (Preventive Care and Screening: Screening for High Blood Pressure and Follow-Up Documented) brings a sigh of relief to DCs, the changes in Medicare’s 2015 fee schedule could mean negative payment for those who did not participate in PQRS reporting in 2013. On Jan.22, 2015, the American Chiropractic Association (ACA) released new resources to help chiropractors with PQRS in 2015.
Here’s a lowdown on the ACA’s most recent recommendations on 2015 PQRS reporting requirements with an aim to provide clarity on payment adjustments and the new fee schedule format.
“It is very important that all DCs who treat Medicare beneficiaries, both participating and nonparticipating, are aware of how the negative payment adjustments affect them when billing claims to Medicare,” said ACA President Anthony Hamm, DC, FACO, in an interview for the website Chiroeco.com.
Background: PQRS applies to all Part B covered services under the Medicare Physician Fee Schedule (PFS). Eligible providers currently participate in the program by submitting documentation related to certain services (or measures).
Calendar year 2015 is the performance period that will affect a provider’s 2017 Medicare reimbursement. If a DC is not able to satisfactorily report the quality measures in the reporting period Jan.1 to Dec.31, 2015, he will face a payment adjustment of 2 percent, i.e. he would get 98 percent of the fee schedule payment instead of the full amount that would otherwise apply for the service.
Reality check: Unfortunately, not all DC’s have taken note. “Some of them have minimal awareness. They need to be on top of things so that they don’t decrease their reimbursement,” opines Doreen Boivin, CPC, CCA, with Chiro Practice, Inc., in Saco, Maine. “If a practice is seeing 25 percent or more of Medicare patients that is a lot of decrease in payment.”
2015 updates in a nutshell: The Chiropractic Coding and Compliance Alert (CHA) has been closely following the developments in PQRS reporting requirements and brings you what matters the most.
Quality Measure #131: Pain Assessment and Follow Up
ACA acquaints us with the fact that presently 131 is incorrectly listed under the Communication and Care Coordination domain in the CY 2015 PFS Final Rule. Since measure 131 was finalized in the CY 2013 PFS Final Rule under the Community and Population Health domain, it therefore actually belongs under the Community and Population Health domain for 2015.
The ACA also recommends that the measure be reported for each visit. Although no diagnosis need be associated with this measure, the documented follow-up plan must be related to the presence of pain. For example, “Patient referred to pain management specialist for back pain” or “Return in two weeks for re-assessment of pain” would meet the documentation criteria.
Change the “pain” pivot: “Sadly, society is focused on PAIN instead of wellness,” laments Boivin. She believes that “people ultimately are coming in because they are in pain or discomfort and the provider is caught having to document that the treatment is improving the pain and overall functionality of the patient.”
This quality measure holds significance as it can help us provide objective data on the impact of pain on the population. According to the American Pain Foundation (2009), approximately 76.5 million Americans suffer from pain. Pain affects more Americans than diabetes, heart disease, and cancer combined.
What it means for you: “For chiropractors to be taken seriously, this documentation is pivotal to show that chiropractic care helps the patient get out of pain and improves overall functionality,” explains Boivin.
Quality Measure #182: Functional Outcome Assessment
ACA suggests that DCs report each visit for patients seen during the 12 month reporting period.
Moreover, remember to keep the functional outcome assessment findings as current as possible.
Even though it is a vital part of evidence-based practice, recent evidence suggests that its use in clinical practices unfortunately is limited, probably “because of the time constraints of a patient visit being 5 to 15 minutes,” suggests Boivin.
With the implementation of quality measure 182, Medicare aims to enhance clinical practice by:
(1) Identifying and quantifying body functions and structure limitations;
Take Note of the PFS Changes
The new format of the 2015 Medicare Fee Schedule is due to the negative payment adjustments to be implemented on all those providers who did not satisfactorily participate in PQRS during the 2013 reporting period. It also applies to providers who were not meaningful users of Electronic Health Records (EHR) in 2014.
Therefore, the payment adjustments apply to all non-participating/non-satisfactorily reporting providers regardless of whether a provider elected to be “participating” (Par) or “non-participating” (Non-Par) for purposes of Medicare payments.
CMS directed all Medicare Administrative Contractors (MACs) to revise the format of their fee schedules to display the limiting charge amount after applying the EHR and PQRS negative adjustment(s).This was done in preparation for the implementation of the negative payment adjustments beginning on January 1, 2015.
Medicare specifically required the MACs to add the following line items:
*Note: DCs are not affected by the Electronic Prescribing (eRx) penalty.
Future implications: Payers of all types are migrating from “pay per service” and toward payment based on the quality of service provided. In fact, these quality measures may become the forerunners of future criteria to prove necessity of care and determine whether providers receive adequate reimbursement. Also, participation in quality measure reporting shows a dedication to the delivery of quality care, thus reassuring patients that their providers are committed to their best interests.
(2) Formulating the evaluation, diagnosis, and prognosis;
(3) Informing the plan of care; and
(4) Helping to evaluate the success of physical therapy interventions.

