Medicare Payment Rates To Increase 1% In 2018
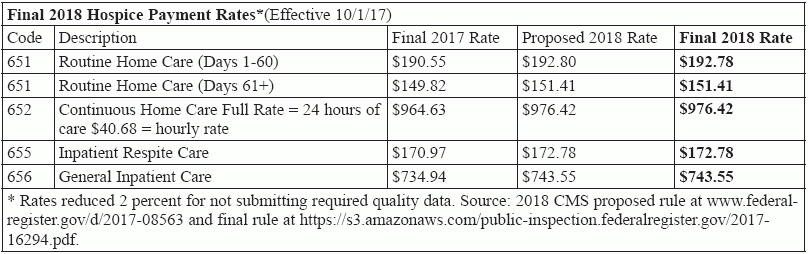
Rates essentially unchanged from proposed rule. No payment surprises unfortunately doesn’t mean no payment headaches in Medicare’s 2018 proposed rule for hospice payment. The Centers for Medicare & Medicaid Services sticks almost exactly to its proposed payment rate increases for the year starting Oct. 1. Rates will increase an average of 1 percent under the rule that CMS released Aug. 1. Slight change: The only change to the rates is a very minor decrease in the Routine Home Care rate for the first 60 days. Instead of $192.80, it will be $192.78 (see chart, p. 67). That’s due to a tiny change in the Service Intensity Add-on Budget Neutrality Factor, from 1.0017 to 1.0018, says the rule published in the Aug. 4 Federal Register. Reminder: CMS makes “SIA payments budget neutral through an annual determination of the SIA budget neutrality factor (SBNF), which will then be applied to the RHC payment rates,” CMS explains in the final rule. “The SBNF will be calculated for each FY using the most current and complete FY utilization data available at the time of rulemaking.” The rate hike will produce a projected $180 million increase over this year’s hospice spending. But the bump is less than half of the 2.1 percent rise hospices saw last year, thanks to a 1 percent cap on hospice pay increases included in the “doc fix” Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) law. Hospices knew the 1 percent increase cap was coming, thanks to MACRA, notes Judi Lund Person with the National Hospice & Palliative Care Organization. There weren’t a lot of changes from the proposed rule, “particularly given that the 1 percent update was pretty much hard-wired by MACRA,” says Theresa Forster with the National Association for Home Care & Hospice. Also as proposed, the aggregate per patient cap amount for FY 2018 will be $28,689.04 — 1 percent more than the current 2017 cap amount of $28,404.99, CMS notes in a release about the rule. The Improving Medicare Post-Acute Care Transformation (IMPACT) Act of 2014 requires the cap amount for accounting years that end after Sept. 30, 2016, and before Oct. 1, 2025, to be updated by the hospice payment update percentage, rather than the Consumer Price Index (CPI), CMS adds. The final rule didn’t add much to the proposed rule for this year’s provisions, Lund Person notes. But it did provide more details for other provisions in the rule, including: Hospice Compare. CMS plans to launch the public quality data comparison site this month, it says in the final rule. As proposed, the Hospice Item Set-based measures will display when the site launches, while the CAHPS-based measures won’t display until this winter. Quality reporting exception. “The rule finalizes the extension or exception for quality reporting purposes from 30 calendar days to 90 calendar days after the date that an extraordinary circumstance occurred,” CMS notes in the release. “This change will align the HQRP with the other post-acute care quality reporting programs, as well as the Hospital Inpatient Quality Reporting Program, and will give additional time for providers to focus on operations related to patient care should a situation arise, such as an unforeseen environmental emergency.” Later than 2018. CMS reviews its discussions and comments it received about potential proposals it will make in later years, including adopting the HEART assessment tool (see story, p. 68) and adding two new quality measures on potentially avoidable hospice care transitions, and access to levels of hospice care. “We’re particularly appreciative that CMS has provided some rich feedback on hospice stakeholder input on planned future changes to the quality reporting program,” Forster tells Eli. “On quality issues, the final rule explained more detail on the development of the two claims-based measures for the two priority areas — burdensome transitions and access to all levels of care — although the measures are still in development,” Lund Person says. “NHPCO was also pleased to see more detail on stakeholder involvement in the development of the Hospice Evaluation and Assessment Reporting Tool (HEART). In general, this final rule provided data analysis and information on issues being considered for future rulemaking rather than new rulemaking for this year.”