Heed Expert Tips For Proper Antipsychotic Medication Coding
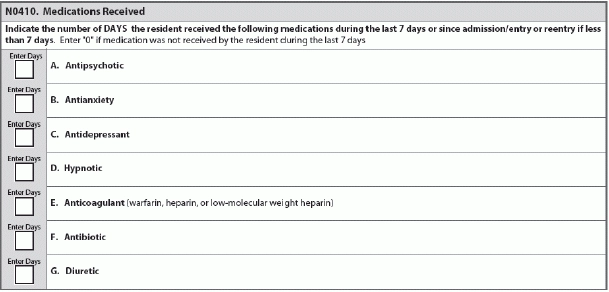
With all the scrutiny that antipsychotic medication use in nursing homes is receiving, you need to keep a close eye on your coding of N0410 — Medications Received, in addition to your quality reporting. Here’s how to avoid making perilous mistakes when you’re reporting antipsychotics on the MDS.
Key: When coding N0410, you need to both review the resident’s medical record and documentation from other healthcare settings where the resident may have received any of these medications. Look for documentation that the resident received any of the medications listed in N0410 during the look-back period.
For N0410A — Antipsychotic, you must record the number of days on which the resident received an antipsychotic medication at any time during the seven-day look-back period, or since admission/entry or reentry if less than seven days.
Important: “For this item, you always want to correctly enter the number of days that the antipsychotic medication was received,” stressed Cheryl Shiffer, RN, MDS Coordinator for the Texas Department of Disability and Aging Services (DADS) in a recent educational presentation. “The correct coding for this item is a number between zero and seven.”
How to Handle the Look-Back Period
This means that if an antipsychotic medication was not used during the look-back period, you would code 0. If the resident received an antipsychotic medication on just one day during the look-back period, you would code 1. And if the resident received an antipsychotic on all seven days, and those seven days fell within the look-back period, you would code 7.
You must code a medication even if the resident received it only once during the look-back period, according to a June 9 presentation by Shirley Boltz, RN, RAI/Education Coordinator for the Kansas Department for Aging and Disability Services (KDADS). You also need to code medications according to therapeutic category and/or pharmacological classification, not based on how the medication was used.
What You Must Include
Include all antipsychotic medications given to the resident via any route, such as orally, intravenously, or intramuscularly, Shiffer instructed. You also must code any antipsychotics given to a resident in any setting (for example, nursing home, hospital, emergency room) while he was a resident of your facility.
What this means: If the resident went to an appointment at the doctor’s office where he received an antipsychotic medication but was not discharged from the nursing home, and then returned to the nursing home, you would code that antipsychotic medication.
Get documentation and evidence that the medication was actually given to the resident when outside the nursing home, Shiffer advised.
When residents receive combination medications, you should code them in all categories/pharmacologic classes that constitute the combination. For example, if the resident receives a single tablet that combines an antipsychotic and an antidepressant (for example, Symbyax®, which combines Zyprexa and Prozac to treat bipolar disorder), then you should code both the antipsychotic and antidepressant categories.
Learn N0410 Coding By Example
The RAI Manual (page N-8) provides the following coding scenario:
Mrs. P’s Medication Administration Record shows that she received risperidone 0.5mg orally once per day on Monday, Wednesday, and Thursday. She also received lorazepam 1mg orally once each day in the morning, as well as temazepam 15mg at bedtime on Tuesday and Wednesday.
How to code: For this scenario, you would code N0410A — Antipsychotic as “3” (risperidone is an antipsychotic medication and was received on three days). Code N0410B — Antianxiety as “7” (lorazepam is an antianxiety medication and was received on all seven days), and then code N0410D — Hypnotic as “2” (temazepam is a hypnotic medication and was received on two days).
Beware: “Administration of these types of medications, particularly in this combination, could be interpreted as chemically restraining the resident,” the RAI Manual states. “Adequate documentation is essential in justifying their use.”