Don't Flush Away Your Urinary Incontinence Coding
Both staff and the resident need to work hard at a toileting program trial, and you need to make sure you’re capturing that effort in your coding of Item H0200 — Urinary Toileting Program.
If you have a resident who is incontinent, you must provide appropriate treatment and services to achieve two goals: to prevent urinary tract infections, and to restore as much bladder function as possible, according to the Oklahoma State Department of Health’s Quality Improvement & Evaluation Service (QIES).
And one way to ensure that your resident is receiving appropriate services is to “develop an individualized, resident-centered toileting program,” QIES instructs.
Give Cognitively Impaired Residents a Chance, Too
Mistake: Don’t overlook residents who have dementia — many residents will respond to a toileting program, especially during the day, QIES says. “Research has shown that one-quarter to one-third of residents will have a decrease or resolution of incontinence in response to a toileting program.”
Important: Still, residents with dementia or other cognitive impairment should meet certain requirements for continence. They should be:
Caveat: But don’t let these criteria box you in. Even if the resident meets none of these four requirements, “a well-developed toileting program where staff toilets the resident prior to episodes of incontinence would be considered a toileting plan,” says Marilyn Mines, RN, BC, RAC-CT, MDS Alert consulting editor and senior manager of clinical services for FROST Healthcare in Deerfield, Ill.
Execute the Toileting Program Properly
First, assess the resident’s bowel/bladder patterns to determine appropriate times to toilet the resident, QIES advises. And second, make sure the resident’s care plan shows that the resident’s toileting program is:
You must follow certain requirements of a toileting program. In addition to a restorative toileting program being organized, planned, documented, monitored, and evaluated, you must ensure that the program is consistent with nursing home policies and procedures, according to a June 3 presentation by Shirley Boltz, RN, RAI/Education Coordinator for the Kansas Department for Aging and Disability Services (KDADS). Also, the program must be consistent with current standards of practice.
And Boltz explained that your documentation must include:
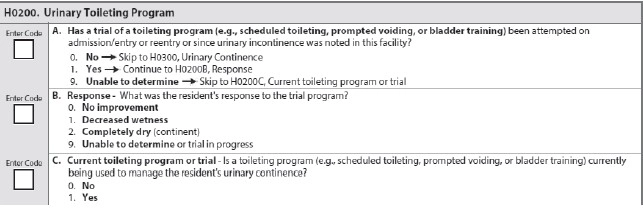
How to Code H0200A
H0200A asks whether the resident has attempted a toileting program trial on admission/entry or reentry or since staff noted urinary incontinence in your facility. In addition to the necessary documentation detailed above, you must also have observations of at least three days of toileting patterns with prompting to toilet, Boltz said. Staff must record the results in a bladder record or voiding diary and evaluation.
Remember: You’re not just tracking the resident’s continence status, Boltz cautioned. Toileting programs must include habit training/scheduled voiding, bladder rehabilitation/bladder retraining, and prompted voiding.
So for H0200A, code 0 — No if for any reason the resident didn’t attempt the toileting program, Boltz instructed. You may need to code this way if the resident is continent with or without toileting assistance, uses a permanent catheter or ostomy, or prefers not to participate in the trial. Then, skip to H0300 — Urinary Continence.
Code 1 — Yes if the resident underwent a toileting program trial at least once or if the trial is in progress. Code 9 — Unable to determine if there’s no documentation in the resident’s record, and then skip to H0200C — Current toileting program or trial.
Understand the Responses for H0200B
If you coded 1 — Yes for H0200A, you will then need to code H0200B — Response to reflect how the resident responded to the trial toileting program. Code 0 — No improvement only if incontinence did not decrease, Boltz said. Code 1 — Decreased wetness if the frequency decreased but the resident is still incontinent (i.e., one less incontinent void per day).
Code 2 — Completely dry if the resident was completely continent of urine. Code 9 — Unable to determine or trial in progress if documentation in the resident’s record is lacking, or if the trial is still in progress.
When You Can Code ‘Yes’ for H0200C
H0200C can be a little tricky to code correctly, especially when a resident isn’t following a toileting program 24 hours per day or during the entire look-back period.
For residents who are currently on a toileting program in the seven-day look-back period, code 1 — Yes for residents who are being managed during four or more days of the seven-day look-back period, according to QIES. Residents must have some type of systematic toileting program, such as bladder rehabilitation/bladder training, prompted voiding, or habit training/scheduled voiding.
Tip: You can still code 1 — Yes even if the resident prefers staff not to wake him at night to toilet but is on a toileting program during the day, QIES adds.
Use This Scenario as a Coding Guide
Boltz provided the following example to illustrate proper coding of Item H0200:
Mr. Smith, who has a diagnosis of congestive heart failure and a history of left-sided hemiplegia from a previous stroke, has had an increase in urinary incontinence. The interdisciplinary team has assessed him for a reversible cause of the incontinence and has evaluated his voiding pattern using a voiding assessment/diary. After completing the assessment, the team determined that they could help Mr. Smith to reduce his incontinence episodes.
The team developed a plan that called for toileting every hour for four hours after receiving his morning diuretic, and then every three hours until bedtime at 9 p.m. The team communicated this approach to Mr. Smith, and the care team has placed these interventions in the care plan. The team will reevaluate the resident’s response to the plan after one month and adjust as needed.
How to code: For this scenario, you would code H0200A as 1 — Yes, and then code H0200B as 9 — Unable to determine or trial in progress. Code H0200C as 1 — Yes.