Are You Performing Discharge Assessments Properly?
Tip: The discharge date must always match the ARD.
Correctly coding discharge assessments can no doubt affect your quality reporting, but also it can greatly impact your survey outcomes — and the Centers for Medicare & Medicaid Services (CMS) is increasing the scrutiny of nursing homes’ discharge assessments. Here are tips on major areas of the discharge assessment process that will help you to stay on track.
Get the Date Right
The first mistake you can make is incorrectly dating the discharge and assessment dates. The discharge date on the MDS 3.0 must be the same date as the Assessment Reference Date (ARD) of the discharge assessment, according to Rabia Khan, MPH, a member of the Quality Measurement and Health Assessment Group at CMS’ Center for Clinical Standards and Quality.
If the discharge date and the ARD are not identical to one another, “that’s a failed area” and the record will be rejected, stated David Malitz, PhD, a statistician with Austin, TX-based Stepwise Systems, in a CMS instructional session.
You must complete the assessment no longer than 14 days after the discharge date, and then you must submit it no more than 14 days after completion, Khan stated in a recent CMS provider update.
Understand the 2 Types of Discharge Assessments
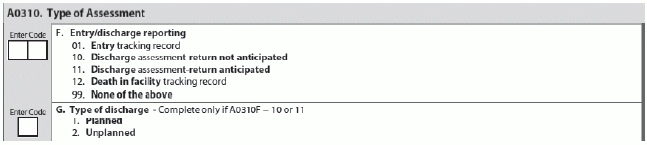
“A0310F is the entry or discharge reporting item, and this indicates there’re five options for whether it’s an entry record; discharge return not anticipated; a discharge return anticipated; death in facility record; or it’s not an entry or discharge record,” Malitz said. “And the entry and the death in facility record are tracking forms only.”
So you essentially have two types of discharge assessments to choose from: “discharge return anticipated” and “discharge return not anticipated.” Complete “discharge return anticipated” when the resident is discharged from the facility and you expect him to return to the facility within 30 days, Khan instructed. “This status requires an entry tracking record each time the resident returns to the facility and a discharge assessment each time the resident is discharged.”
Example: You would mark the resident status as “discharge return anticipated” when the resident is discharged to a hospital or other setting, such as a respite resident, who comes in and out of the facility on a relatively frequent basis, Khan noted. This is true unless, of course, you don’t anticipate the resident’s return within 30 days.
“Don’t include leaves of absence or if a resident is sent to the hospital for observation but not admitted,” Malitz warned. “If the resident is returning from therapeutic leave of absence or hospital observation, that’s a continuation of the Medicare Part A stay.” And you can obtain this information from medical admissions or transfer records.
However, if the resident is out of the facility for greater than 24 hours on an LOA or observation stay, you must complete a discharge assessment. (RAI Manual 2-10 – 2-11: “Any of the following situations warrant a Discharge assessment, regardless of facility policies regarding opening and closing clinical records and bed holds: … resident has a hospital observation stay greater than 24 hours, regardless of whether the hospital admits the resident.”)
You would complete the discharge assessment “return not anticipated” when the resident is discharged and is not expected to return within 30 days. “For instance, if a resident was discharged to home or to an assisted living facility, this would be the correct type of discharge to complete,” Khan said.
Caveat: But if the discharged resident returns within the 30-day period, you “would begin the assessment process over again with an admission assessment after completing an entry tracking record signifying that the resident is an ‘admission,’” Khan noted.
Important: “A key point to remember when determining the type of discharge assessment needed is that nursing home bed hold status and opening and closing of the medical record have no effect on these requirements,” Khan stated.
How to Code Planned Vs. Unplanned Discharges
In addition to “return anticipated” or “return not anticipated,” discharges are also categorized as “planned” or “unplanned” under A0310G Type of Discharge. You need to complete this subsection only if you selected discharge assessment-return not anticipated (10) or –return anticipated (11) in A0310F.
“An unplanned discharge includes, for example, acute-care transfer of the resident to a hospital or an emergency department in order to either stabilize a condition or determine if an acute-care admission is required based on emergency department evaluation,” Khan explained. An unplanned discharge could also include a resident who unexpectedly leaves the facility against medical advice or unexpectedly decides to go home or to another setting.
Keep in mind: If the resident is admitted to the hospital or remains in an observation stay longer than 24 hours, you must perform a discharge assessment at that point, Khan said. Likewise, for unplanned discharges, you must complete the discharge assessment to the best of your abilities. You can use a dash when you’re “unable to determine the response to an item, including the interview items,” she noted.
“In a stand-alone discharge assessment, there will be no interview items; however, if combined with another assessment type, there may be,” Khan said. “In some cases, the facility may have already completed some items of the assessment and should record those responses or may be in the process of completing an assessment.” You can then combine the discharge assessment with other assessments when you’ve met the requirements for all assessments.
For planned discharges, you should schedule the discharge assessment proactively and complete it in the same manner as any other assessment, Khan said. Although fewer interview items are required in the discharge assessment, you should consider those that are required as a priority.
Warning: But don’t expect to get away with using dashes in a planned discharge situation. “It is expected that the need to use a dash on the planned discharge would be infrequent and rarely encountered,” Khan cautioned.