Get the Skinny on Feeding Assistants
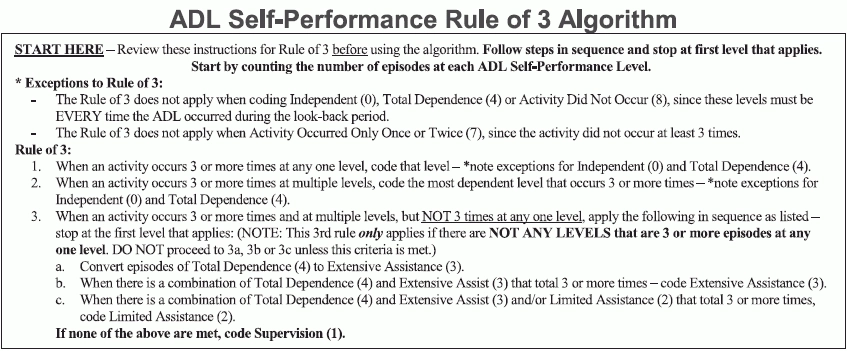
Check in to make sure your facility is employing the correct standard of care in the dining room — and earning the reimbursement your facility deserves. Feeding assistants are a crucial part of some of your residents’ daily life. Fully understanding the different categories of assistance — particularly how assistants are paid — is key to understanding how to best code both Section G (Functional Status) and Section GG (Functional Abilities and Goals). Surveyors are interested in observing how facilities handle residents’ specialty diets (and determining exactly what constitutes a specialty diet), as well as making sure that staff confidently and knowledgably document exactly which team members are involved in each resident’s daily life. Beware: Look in Appendix PP for the specific guidance; the Ftag you need to look out for is F811. “If the feeding assistant is paid by the facility, the individual would count as far as coding for Section G — just remember you also have to include in your assessment any other staff that participated in the resident receiving nutrition (except medication administration),” says Jane Belt, Rn, Ms, RaC-Mt, RaC-Ct, QCP, curriculum development specialist at AANAC in Denver, Colorado. Prioritize Safety The current survey regulations on feeding assistants are focused on keeping residents safe. In terms of feeding assistants, your facility should ensure that anyone employed and on staff is under direct medical supervision. The Centers for Medicare and Medicaid (CMS) requires all paid [employed] feeding assistants to complete a state-approved training course. Historically, the quality of help that feeding assistants provide has been lacking. Even with the great strides facilities have made — and regulations and policies have forced — there is frequently room for improvement, in both helping residents and earning the reimbursement you deserve. Both the MDS and the clinical record should support consistent documentation that a resident who needs a feeding assistant’s help does not have a complicated feeding problem (see Appendix PP guidance, below, for exactly what constitutes a complicated feeding problem). Different states have different guidelines and regulations for paid feeding assistants. For example, Wisconsin state law allows facilities to employ staff as young as 16 years old in this role, assuming all other employment and training requirements are met. Check out the exact language on current Appendix PP guidance on feeding assistants, as summarized in F811 guidance, below: “§483.60(h) Paid feeding assistants-§483.60(h)(1) State approved training course. A facility may use a paid feeding assistant, as defined in §488.301 of this chapter, if- (i) “The feeding assistant has successfully completed a State-approved training course that meets the requirements of §483.160 before feeding residents; and (i) “A facility must ensure that a feeding assistant provides dining assistance only for residents who have no complicated feeding problems. Code Accurately When a resident needs consistent feeding assistance, you must document the need in the resident’s comprehensive care plan (CAA), as mentioned above, but also in Section G (Functional Status) in the MDS. To code feeding assistance accurately in item G0110 (Activities of Daily Living (ADL) Assistance), you’ll need to follow the RAI Manual’s algorithm and helpful visual flowchart. The current iteration of the RAI Manual (Version 1.16), which goes into effect this Oct. 1., provides even more explicit guidance than before on how to evaluate and code activities of daily living (ADL) self-performance. See the algorithm instructions below and consult the flowchart on page G-8. Remember: A resident’s family or other visitors may arrive at mealtimes to spend time together with their loved one. Even if a resident’s daughter shows up every day and helps at dinner, this would not be included in the MDS coding calculation because the assistance is not provided by a paid feeding assistant. By all means document the daughter’s visitation and help — and note whether the assistance is clinically appropriate. If a resident requires feeding assistance and the daughter is informally filling in, consider a conversation with the interdisciplinary care team on evaluating the comprehensive care plan and a way forward to ensure that mealtime remains safe.
(ii) “The use of feeding assistants is consistent with State law.
§483.60(h)(2) Supervision.
(i) “A feeding assistant must work under the supervision of a registered nurse (RN) or licensed practical nurse (LPN).
(ii) “In an emergency, a feeding assistant must call a supervisory nurse for help.
§483.60(h)(3) Resident selection criteria.
(ii) “Complicated feeding problems include, but are not limited to, difficulty swallowing, recurrent lung aspirations, and tube or parenteral/IV feedings.
(iii) “The facility must base resident selection on the interdisciplinary team’s assessment and the resident’s latest assessment and plan of care. Appropriateness for this program should be reflected in the comprehensive care plan.”