What CMS Wants You To Understand About The New Section GG
Find out what the term ‘helper’ really means for your coding.
If you’re nervous about coding the new Section GG — Functional Abilities and Goals beginning on Oct. 1, you’re not alone. But now you can glean new insights from the Centers for Medicare & Medicaid Services (CMS) on the most important instructions you need to know.
CMS finalized the Item Sets for v1.14.1, effective Oct. 1, 2016 and posted them on Aug. 10 on the MDS 3.0 Technical Information webpage (www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/NHQIMDS30TechnicalInformation.html). While the RAI Manual v1.14 is still in a “draft” version, the fact that CMS finalized the item sets means you shouldn’t expect anything but very minor revisions in the final version.
Good news: CMS also released a series of four training videos that focus on coding Section GG (go to www.youtube.com/user/CMSHHSgov/videos). The videos are divided into bite-sized pieces and provide a solid overview of the new section, with tips, definitions, and coding scenarios. Here are some of the highlights.
Pay Attention to the Timeframes
“The timeframes associated with this section are really important to understand,” stressed Terri Mota, BSN, RN, CALA, nurse consultant with the CMS Quality Measurement & Value-Based Incentives Group within the Division of Chronic and Post-Acute Care, in the instructional video.
Significance: “We’re trying to get an understanding of the resident’s status at admission, which is a baseline assessment that reflects the resident’s usual performance at the time of admission” and their status at discharge, Mota explained. “As well as an understanding of their discharge goals which are established at the start of the SNF stay and are related to self-care and mobility performance.”
For GG0130 — Self-Care and GG0170 — Mobility, the assessment period for the admission performance in Column 1 is Day 1 through Day 3 of the SNF PPS stay, beginning with the date coded in A2400B — Start date of the most recent Medicare stay.
When you capture self-care and mobility items on discharge to reflect the resident’s status at the end of the SNF PPS stay, the assessment period is the last three days of the stay, ending on the date in A2400C — End date of the most recent Medicare stay.
Understand the New Term ‘Helper’
Important: Although the term “helper” is new, the definition of it is consistent with the definition of facility staff in Section G — Functional Status. For the purposes of completing Section GG, a “helper” is defined as facility staff who are direct employees or facility-contracted employees (for example, rehabilitation staff and nursing agency staff).
The definition does not include individuals hired, compensated or not, by individuals outside of the facility’s management and administration, such as hospice staff, nursing students or CNA students, and so on, Mota said. “Therefore, when helper assistance is required because a resident’s performance is unsafe or of poor quality, only consider facility staff when scoring the amount of assistance provided.”
Example: You’re coding item GG0130A — Eating for Mr. Haywood, who has a swallowing problem. Although he can eat, he often eats too quickly which is unsafe considering his swallowing problem.
So to ensure that Mr. Haywood is safe while eating, a staff member sits with him to provide direct supervision and cue him to slow down — this staff member is the helper.
But if Mr. Haywood’s daughter visits each day at lunch and dinner, any assistance she provides for him while he eats and drinks doesn’t count. You can’t consider the daughter’s assistance when scoring this item, Mota cautioned.
Code the Resident’s ‘Usual’ Performance
When coding Section GG, always keep in mind that you’re not aiming to code the resident’s most dependent or independent level of performance during the assessment period. Instead, you should code the resident based on his “usual performance,” or baseline performance, which is the resident’s usual activity or performance of the self-care or mobility activities.
Rule of thumb: “Therefore, if there’s fluctuation in the performance of activities during the three-day assessment, the performance wouldn’t be the worst, and it wouldn’t be the best, but it would be what’s ‘usual’ for that individual,” Mota noted.
How to Set Discharge Goals
In Column 2 of GG0130 and GG0170 — Mobility, you need to code the discharge goals for each activity. But where can you find the information you need to code the discharge goals?
Crucial: “Licensed clinicians can establish a resident’s discharge goals at the time of admission based on discussions with the resident and family, professional judgment and the professional’s standard of practice,” Mota stated. Ultimately, you need to look to the resident’s care plan to find the correct coding for Column 2.
Although you may have residents who will have discharge goals that show improvement from their usual performance that you code in Column 1 upon admission, that won’t always be the case. Don’t worry if your coding of a particular activity shows the same, or even slightly declining, ability for Column 1 and Column 2.
Examples: On admission, you code a resident’s eating in GG0130A as 03 — Partial/moderate assistance. Based on the team’s assessment, including input from the resident, you expect that the resident’s performance will improve such that he will require only minimal setup help, Mota illustrated.
In this case, you would code Column 2 as 05 — Setup or clean-up assistance. This would show that you expect a functional improvement.
But in some cases the goal may be to simply maintain the resident’s performance. For instance, a resident’s usual performance coded in Column 1 for GG0130B — Oral hygiene is 02 — Substantial/maximal assistance, and the resident has a progressive degenerative condition.
The team and resident feel that, although the resident isn’t expected to gain function regarding oral hygiene, maintaining function is desirable and achievable as a discharge goal. So in this case, you would code the discharge goal for GG0130B in Column 2 as 02, the same coding as Column 1.
In yet another case, the care plan’s goals may not even be to maintain function, but instead to slow the decline as much as possible, even though a decline is still expected. For instance, a resident’s admission performance for GG0130C — Toileting hygiene is 04 — Supervision or touching assistance, but the resident’s functional decline and goal of slowing that decline may result in a discharge goal of 03 — Partial/moderate assistance, which is lower than the admission performance code.
Avoid These Coding Missteps at All Costs
Important: Although you can use codes 07 — Resident refused, 09 — Not applicable, and 88 — Not attempted due to medical condition or safety concern for Column 1, you cannot use them when you’re coding the discharge goals in Column 2, because they “are not appropriate code responses for these goals,” “Only use the six-point scale (independent through dependent) to code the resident’s discharge goals.”
Caution: The use of 09 — Not applicable is not arbitrary, warns Marilyn Mines, RN, BC, RAC-CT, MDS Alert Consulting Editor and Senior Manager at Marcum LLP in Deerfield, Ill. This response has “a very specific definition that isn’t indicated on the MDS item set itself, but must not be forgotten.”
According to the draft RAI Manual, you should code “not applicable” only if the resident didn’t perform the ADL “prior to the current illness, exacerbation, or injury.” In other words, you must know what the level of functioning for this activity was prior to the most recent hospitalization.
And whatever you do, don’t use dashes for the Section GG items. Using dashes could result in a 2-percent reduction in your facility’s annual payment update. Instead, use 07, 09, or 88 (just not for the discharge goals).
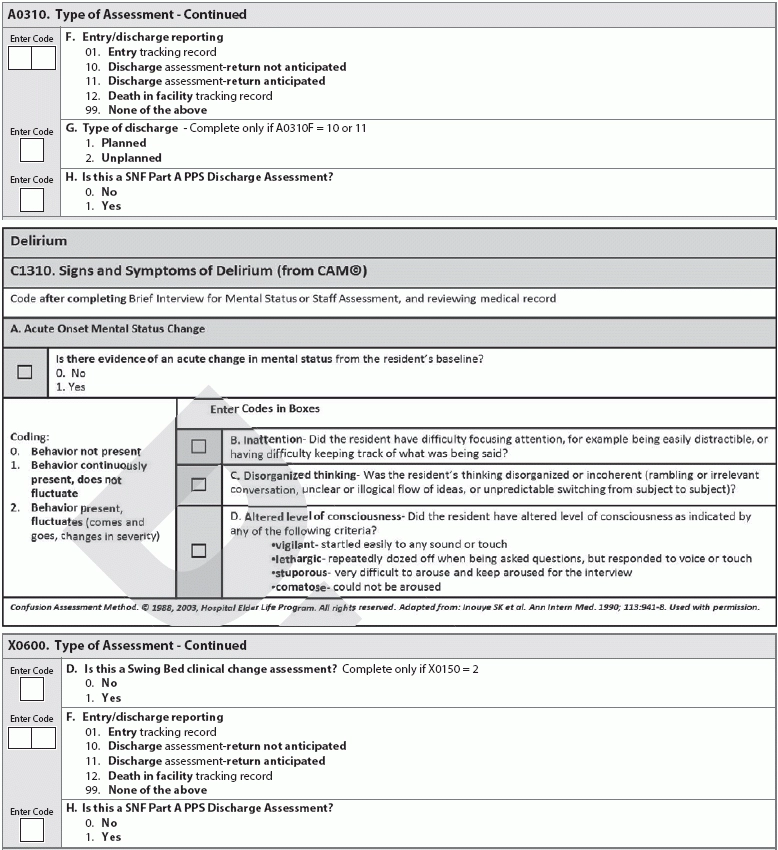
Don’t forget: With all the attention on the new Section GG items, don’t overlook the other new items and significant changes. For instance, the MDS will now include the new sub-items, A0310H — Is this a SNF Part A PPS Discharge Assessment? and X0600H — Is this a SNF Part A PPS Discharge Assessment?
Also, CMS deleted items C1300 — Signs and Symptoms of Delirium and C1600 — Acute Onset of Mental Status Change, replacing them with the new item C1310 — Signs and Symptoms of Delirium (from CAM©).
Resources: To access the draft RAI Manual and finalized item sets, go to www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/MDS30RAIManual.html. Scroll down to the “Related Links” section at the bottom of the webpage.