Learn How All Team Members Can Observe ADLs For Minor Changes, First
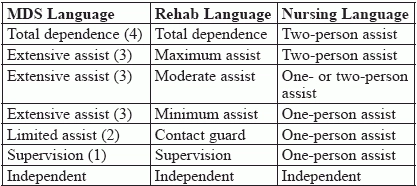
Use your colleagues’ experiences and observations to maximize your care. Teamwork is the only way to provide care for a resident in a SNF. You can’t be everywhere at once, so you rely on your team members to assist residents, as well as to observe what’s going on. However, you may have totally different training from your team members. And the language you used to describe care in nursing school is different from what your colleague learned during his physical therapy education. Learn how to translate team members’ observations into what you need to know to complete the MDS. You and your team members frequently assess mobility. Recording your observations accurately and in a timely manner is essential, but so is understanding what you each mean. When you speak the same language, it’s easier to establish a timeline of each resident’s mobility and function, and to better your team’s assessments, coding, and care. Start Talking the Same Language Consider how you document ADLs for Section G (functional status). Item G0110 (Functional status: Activities for daily living) includes mobility activities like bed mobility and transfers. Bed mobility takes three situations into consideration: moving a resident to and from a horizontal, lying position (getting a resident in and out of bed); turning a resident in bed; and positioning a resident in bed. Each discipline has its own way of describing the steps in this process. Here’s a breakdown that shows how descriptive language varies for the MDS, rehab therapists, and nurses from Renee Kinder Ms CCC-sLP RaC-Ct, director of clinical education at encore Rehabilitation services: Note these PT/OT Details If a resident is receiving occupational or physical therapy, keep an eye out for changes in function through therapists’ observations. Understanding the variations in phrasing between these two disciplines will help you narrow in on your patient’s ability. For example: PT words and phrases like “rolling right, rolling left, scooting, bridging, supine to sit, sit to supine” translate into the MDS language of the ease with which a resident gets into bed (or into a lying position), how the resident moves from side to side, and the resident’s positioning while in bed (or alternate sleep furniture). PT notes along the following lines, as described by Kinder, show the subtle changes in bed mobility that staff can document across the clinical record, which you will use in your assessment in Section G: Don’t miss: If a normally mobile resident is, for the past week, reluctant to get out of bed because of pain, but ultimately manages — with weight-bearing support of his legs from one staff member, you’d code across multiple sections. Code like this: Code these observations in: Be sure to note whether the pain is temporary or specific to the movements needed to transfer from a horizontal position to upright. Encourage team members to record any changes in the recurrence or amount of assistance needed in other transfers, such as toilet transfers. Remember: Because you’re relying on busy team members’ observations and experiences, and because notes aren’t always written or legible, it’s also helpful to gather the information you need to complete the MDS from conversation. Residents may not be able to articulate any changes that they’re experiencing, which is why observations from all involved team members are crucial for accurate ADL assessment. Talk to your CNA team members to evaluate bed mobility and dressing, using specific, probing questions. Example Conversation: (From the RAI Manual) RN: “Describe to me how Mrs. L. moves herself in bed. By that I mean once she is in bed, how does she move from sitting up to lying down, lying down to sitting up, turning side to side and positioning herself?” CNA: “She can lay down and sit up by herself, but I help her turn on her side.” Following this conversation, code G0110A using the following: 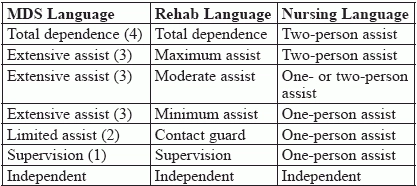
RN: “She lays down and sits up without any verbal instructions or physical help?”
CNA: “No, I have to remind her to use her trapeze every time. But once I tell her how to do things, she can do it herself.”
RN: “How do you help her turn side to side?”
CNA: “She can help turn herself by grabbing onto her side rail. I tell her what to do. But she needs me to lift her bottom and guide her legs into a good position.”
RN: “Do you lift her by yourself or does someone help you?”
CNA: “I do it by myself.”
RN: “How many times during the last 7 days did you give this type of help?”
CNA: “Every day, probably 3 times each day.”