How You Can Better Understand Resident Goal Setting
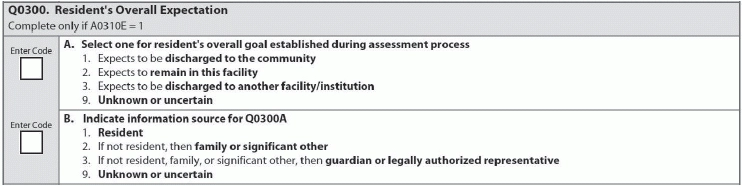
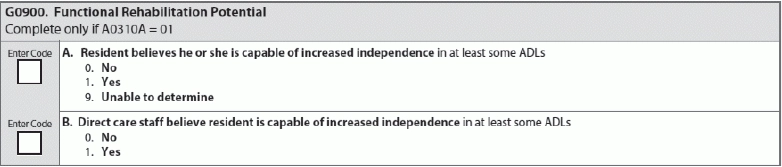
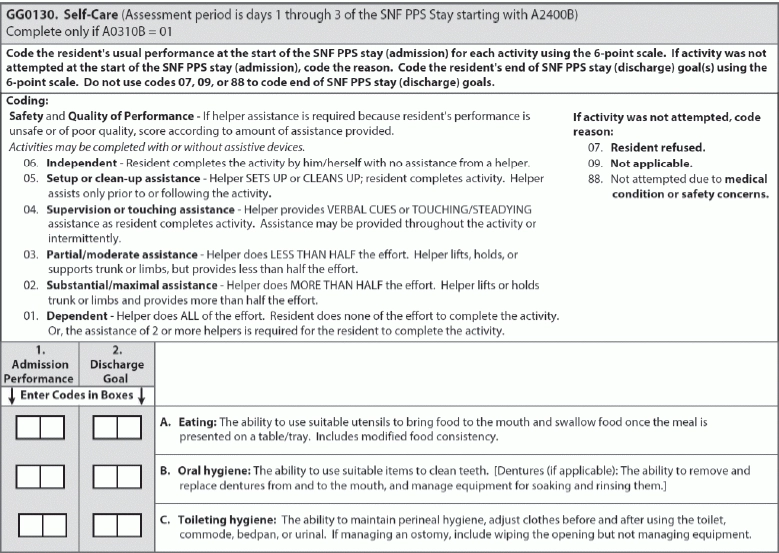
Recording residents’ wishes and coding resident goals across the MDS. Section GG is still new enough to be confusing, and you may have trouble applying your initial conversations with residents to the MDS, especially when learning a resident’s expectations and setting goals. Questions you ask for Section Q yield answers you need to code items in Section G and Section GG. Example: A resident was just admitted who already expresses wishes to leave the facility. You’ve had residents over the years who complain about having to leave home and otherwise mourn their dependence, but this resident is adamant that he “wants out. Now.” He seems to have a supportive family and the resources to manage once discharged, but you’re worried that the level of care that he needs is beyond what he’d receive in his daughter’s home or his own apartment. How do you code Q0300 (resident’s overall expectation) when you don’t agree? Would you record these wishes elsewhere in the MDS as well? Listen to the Patient: Make sure the resident is at the center of any conversation and, ideally, driving the conversation and goal-setting. The resident’s family can be a part of this conversation and you’ll need to be careful to accurately record their level of involvement on the MDS. Know these Q0300 Basics Q0300 is applicable only during admission or readmission. Remember that you’re recording the resident’s wishes in this item. As this resident wishes to leave, you’d code 1 — Expects to be discharged to the community for Q0300A (… resident’s overall goal established during assessment process). If your conversation and assessment include only the resident, you’d code 1 (resident) for Q0300B (Source of information for resident’s overall expectation). Code 1 even when the resident’s family is present if the resident voices his wishes; code 2 (Resident’s family or significant other) if the resident’s family say he’ll be discharged but you don’t hear it from the resident himself. Remember: The RAI Manual considers Section Q “individualized and resident-driven,” meaning that the resident’s wishes matter, rather than “what the nursing home staff judge to be in the best interest of theresident.” Q0300 (Resident’s overall goal established during assessment process) should focus exclusively on the resident’s expectations, regardless of whether staff considers these expectations realistic. “We are responsible for listening to and hearing what the residents’ wishes and desires are, as long as they have not been adjudicated as being incompetent. With that as our first priority, we are also charged with helping the resident, through the care-planning process, to meet their goals,” Marilyn Mines, Rn, BC, RaC-Ct, senior manager at Marcum LLP, says. Go further: Your conversations about goal-setting, in terms of the resident desiring discharge from the facility, has implications elsewhere in the MDS. Sections G (Functional Status) and GG (Functional Abilities and Goals) focus on goal-setting, and you can use the information you’ve gleaned to code these as well. For example: If you’re assessing that the resident needs to become a bit steadier on his feet to live safely outside of the SNF, code 1 (Yes) for G0900A (Resident believes he or she is capable of increased independence in at least some ADLs). In scenario above, you’re concerned about a resident thriving without assistance. Think about how a resident would fare with the intensive physical and occupational therapies, if the resident is set to receive these therapies while living at your facility. In physical and occupational therapy, the resident will complete exercises and learn modifiable movements that should provide added strength and agility. A therapist may suggest a mobility device that could make a big difference, too, such as switching to a different cane that could make ambulation safer and easier for the resident. A resident who is still walking with the assistance of a cane and wants to improve her confidence and ability to move around is a resident with a realistic goal. If this is the case, code G0900B (Direct care staff believe resident is capable of increased independence in at least some ADLs) as 01 (Yes). When planning discharge, “referrals to local contact agencies, therapeutic home visits and assessments, and social service interventions are approaches to be implemented during this process,” Mines says, The RAI Manual states: “Each care plan should be individualized and resident-driven. Whenever possible, the resident should be actively involved, except in unusual circumstances such as if the individual is unable to understand the proceedings or is comatose. Involving the resident in all assessment interviews and care planning meetings is also important to address dignity and self-determination survey and certification requirements.” (CFR §483.15 Quality of Life) Code Self-Care Goals in Section GG, too Don’t forget: You can also use this conversation (and your assessment over the first three days) to code Section GG (Functional Abilities and Goals). Make sure, in your conversation, you find out whether the resident expresses a wish to live independently or thinks he will have assistance in the form of a family member or a hired aide, as the answer will affect how you code GG0130 (Self-Care). Tricky: You know Section GG is new, and figuring out when to code what is still a little confusing for everyone. Item GG0130 is especially confusing because of the language — it’s unclear when the goals are supposed to be set, recorded, and met. Here’s a breakdown: “We have to set at least one goal within three days of admission. When the resident is discharged, we have to record whether the goal was met or if there has been progress toward the goal. First we set a goal, then we determine how well we did at meeting that goal,” Mines says. For admission performance, you must use your own assessment to complete GG0130A1 (Admission assessment for Self-Care: Eating), GG0130B1 (Admission assessment for Self-Care: Oral Hygiene), and GG0130C1 (Admission assessment for Self-Care: Toileting). These levels ranging from 05, which indicates that the resident needs help with mere setup and cleanup, to 01 for a resident who is completely dependent on assistance include: GG0130 (Self-Care) documents current realities and goals for eating, oral hygiene, and toileting. If the resident hopes to live completely independently at discharge, code GG0130A2 (Discharge Goal: Eating), GG0130B2 (Discharge Goal: Oral Hygiene) and GG0130C2 (Discharge Goal: Toileting Hygiene) all as 06 (Independent). If the resident knows he will have assistance, you will need to gauge how much he help he will need before you can accurately code for assistance. The values you use for this item are those listed above for the admission assessment — 05 for a resident who needs help with just setup and cleanup down to 01 for a resident who is completely dependent. Best Care Practices: If you’re still unsettled, plan a bigger conversation, Renee Kinder Ms CCC-sLP RAC-CT, director of clinical education at Encore Rehabilitation services, suggests. “In this situation, we would move to patient-centered care planning, which includes informed consent. I would recommend all applicable interdisciplinary team members be present to educate the patient and family members of risks,” Kinder says. For example: Suppose your resident desires to return home to his previous living situation, but you still deem him at an increased risk for falls secondary to unsteady gait pattern. “Team members needed to educate the patient may include the physical therapist, MD, and nursing teams,” Kinder says. “Then the team collectively develops a comprehensive discharge care plan to honor to patients wishes.”