Get The Answers To 3 Section M Coding Problems
How to avoid downstaging when you have reopening of healed ulcers.
Coding blisters, pressure-relieving beds and reopened pressure ulcers are just a few of the tricky areas of Section M — Skin Conditions. Let the MDS experts guide you in the right direction with these problems and solutions.
How to Code M0700 for a Blister-Type Pressure Ulcer
Problem: How should I code item M0700 — Most Severe Tissue Type for Any Pressure Ulcer when a resident’s pressure ulcer presents as a blister?
Solution: “Pressure ulcers sometimes present as blisters, particularly in the heel area,” noted Jeffrey M. Levine, MD, a specialist in geriatric medicine and wound care, in a recent blog posting on his website (www.jeffreymlevinemd.com).
If the resident has a blister that is filled with clear serous fluid, you would code it in M0300B — Stage 2 Pressure Ulcers, Levine instructed. If the ulcer presents as a blood-filled blister, you would code it in M0300G — Unstageable Pressure Ulcers Related to Suspected Deep Tissue Injury.
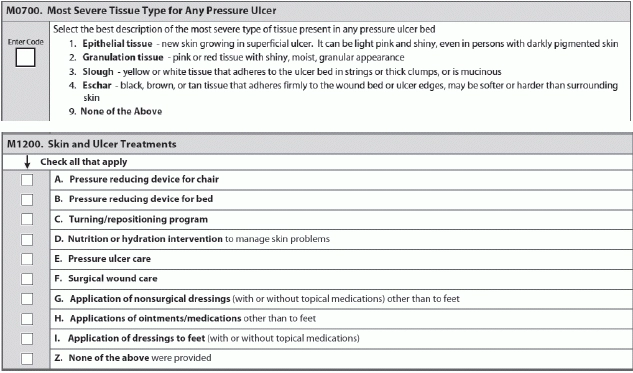
When you’re coding M0700, you have four choices: epithelial tissue; granulation tissue; slough; or necrotic tissue (eschar). “Epithelial tissue refers to the closely packed cells that cover the entire surface of the body, and separated from underlying tissue by a thin sheet of connective tissue which provides structural support and binds to neighboring structures,” Levine explained.
So wound healing “is characterized in part by the process of epithelialization, which occurs when fresh epithelial cells proliferate and spread over the open wound bed, providing cover for the wound and forming new skin,” Levine stated. Therefore, when coding a blister in M0700, the correct answer is 1 — Epithelial tissue.
Why Nice Beds Don’t Equal M1200B Coding
Problem: All of our facility’s beds are pressure-relieving, pressure-reducing, or pressure-redistributing, so should we check the box for M1200B on every MDS for every resident?
Solution: The short answer is no, said Carol Siem, MSN, RN, GNP-BC, RAC-CT, in a recent article for the Quality Improvement Program for Missouri (QIPMO) newsletter. Not all of your residents have skin health problems, and you should base your coding of M1200 — Skin and Ulcer Treatments on the individualized needs of each resident.
“We do have residents who are very low-risk for developing a skin problem,” Siem noted. “Having a higher quality mattress on all our beds is one way of providing quality care and reduces the potential for developing skin issues.”
But that doesn’t mean you can code M1200B — Pressure reducing device for bed for all residents, regardless of their existing or potential for skin problems. “The key is if a problem develops, then we must assess those residents’ particular needs and let that guide us to more individualized and specific interventions,” Siem added.
Don’t Be Tempted to ‘Downstage’ Healed Ulcers
Problem: How do I code a superficial reopening of a healed Stage 4 pressure ulcer?
Solution: When a Stage 4 pressure ulcer heals, you must document it in the MDS as a “healed Stage 4” in M0900 — Healed Pressure Ulcers, Levine said. And if the ulcer reopens — even if the reopened area is superficial and looks like a Stage 2 pressure ulcer — you would document it as a “reopened Stage 4.”
Remember: “The RAI Manual prohibits ‘back staging’ (also called reverse staging or downstaging) of pressure ulcers as they heal,” Levine stressed. So if you coded this reopened ulcer as a Stage 2, you would effectively be downstaging from a “healed Stage 4” to a Stage 2, which is prohibited.