Overcome 3 Pressure-Ulcer Staging Stumbling Blocks
Make sure you’re not coding these types of wounds as ‘worsening.’
There’s no doubt that the Centers for Medicare & Medicaid Services (CMS) is eager for you to improve the accuracy of your pressure-ulcer coding. Here are three of the biggest problems that your peers tend to struggle with when coding Section M — Skin Conditions.
1. Take the Sting Out of Coding Blisters
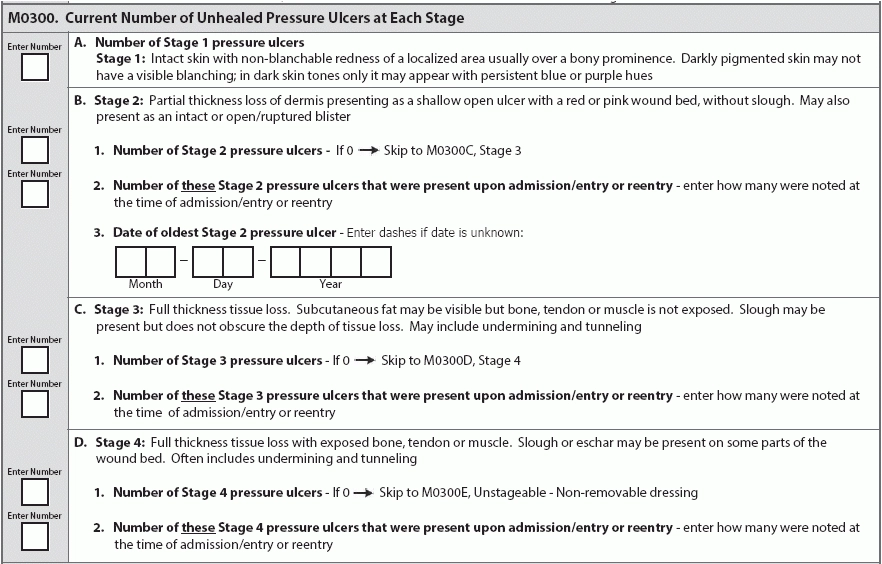
“The presence of blisters presenting as a pressure ulcer is in the RAI Manual as well as in the NPUAP definitions,” noted elizabeth ayello, PhD, Rn, aCns-BC, CWon, etn, MaPWCa, Faan, in a CMS training session. For Stage 2 pressure ulcers, the RAI Manual specifically notes that the ulcer “may also present as an intact or open/ruptured blister.”
Upside: Here, CMS gave long-term care the flexibility to take a holistic approach to blister pressure ulcers, “because quite honestly, there is very little quantifiable research and evidence out there on blister pressure ulcers,” Ayello said. So by the RAI Manual indicating that you need to look at not just the color of the fluid in the blister, but also what’s going on with the skin around that blister pressure ulcer.
Do this: CMS tells you to examine the skin around the blister pressure ulcer to look for signs of deeper tissue damage, such as color changes, tenderness, bogginess, firmness, or warmth or coolness. These signs indicate a suspected deep tissue injury (sDTI), which you would code in M0300G — Unstageable – Deep tissue injury, rather than a Stage 2 pressure ulcer (M0300B).
Why is this important? Because if you stage a wound as a Stage 2 pressure ulcer, but it was really an sDTI, and then it opened up and became a Stage 3 or 4, “now you have a situation where you have a worsened pressure ulcer,” Ayello warned.
2. Untangle Stage 3 vs. Stage 4
Problem: Data suggests that clinicians tend to do well when identifying Stages 1 and 2 pressure ulcers, but that competency level drops off dramatically when you reach Stages 3 and 4, Ayello noted.
Stage 3 pressure ulcers involve full-thickness tissue loss with possible subcutaneous fat visible but no exposed bone, tendon, or muscle. Some slough may be present, but it shouldn’t obscure the depth of tissue loss, and there may be undermining or tunneling.
The key here is that if you see any other structures in the wound other than subcutaneous tissue, you don’t have a Stage 3 pressure ulcer, you have a Stage 4, Ayello said. So be sure that you don’t have bone, tendon, or muscle visible or directly palpable.
Stage 4 pressure ulcers have full-thickness tissue loss with exposed bone, tendon, or muscle, and slough or eschar may be present on some parts of the wound bed. You may often have undermining and/or tunneling. Stage 4s can extend into muscle and supporting structures like the fascia, tendon, or joint capsule, with the possibility of osteomyelitis.
Important: Keep in mind, however, that the depth of a Stage 4 pressure ulcer can vary by the anatomical location, depending on the depth of the subcutaneous tissue. For instance, there’s far more subcutaneous tissue on the buttocks than other parts of the body, with no subcutaneous tissue on the ear, bridge of the nose, occiput, and malleolus. So in these parts of the body, remember that cartilage serves the same anatomical function as bone and so you should classify a pressure ulcer with exposed cartilage as a Stage 4.
3. What to do When Unstageable Becomes Stageable
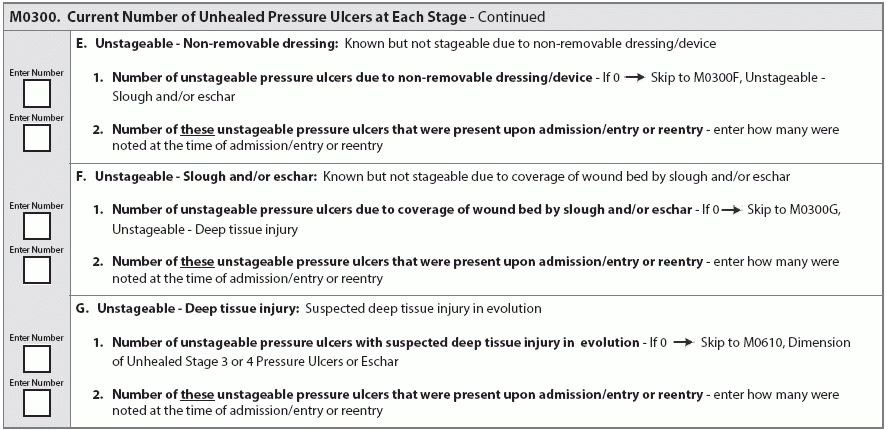
If a resident has a cast or other non-removable dressing or device under which you know he has a pressure ulcer, you need to code it in M0300E — Unstageable – non-removable dressing. But once the cast comes off, you can then stage the pressure ulcer numerically.
The same goes for other situations where you cannot see the anatomical tissue and therefore cannot stage the pressure ulcer, like for M0300F — Unstageable – Slough and/or eschar.
Example: Upon admission, a resident presents with an unstageable pressure ulcer due to slough and/or eschar, so you code the wound accordingly as unstageable (M0300F). The clinician debrides the wound to remove the slough and/or eschar, revealing enough of the tissue to determine the anatomical depth of soft tissue damage.
There is still some slough, but you can clearly see muscle and tendon exposed in the wound. So then on the subsequent MDS record, you would reclassify this pressure ulcer and code this it as a Stage 4 (M0300D). But this is not a worsening pressure ulcer, and you would still code the Stage 4 as present on admission.
This is true for any unstageable pressure ulcer that becomes stageable. The RAI Manual states: “If a pressure ulcer was unstageable on admission/entry, do not consider it to be worsened on the first assessment that it is able to be numerically staged.”