Deep Dive: Launch Yourself Into Falls With Major Injury QM
Brace yourself for J1900 coding to become a much higher-stakes endeavor.
The thought of a resident having a fall that results in an injury will surely give you chills. After all, falls with major injury impact your quality measures (QMs), Five-Star Rating, survey compliance, and the Quality Reporting Program (QRP) data, at the very least.
“We all recognize the concern that providers experience when any resident falls, knowing that falls are a leading cause of morbidity and mortality,” notes Jane Belt, Ms, Rn, RaC-Mt, QCP, Curriculum Development Specialist for the American association of nurse assessment Coordination (AANAC).
The Centers for Medicare & Medicaid Services (CMS) has also noted that previous falls are in indicator for future falls. CMS continues to make fall reduction a top priority, and so should you.
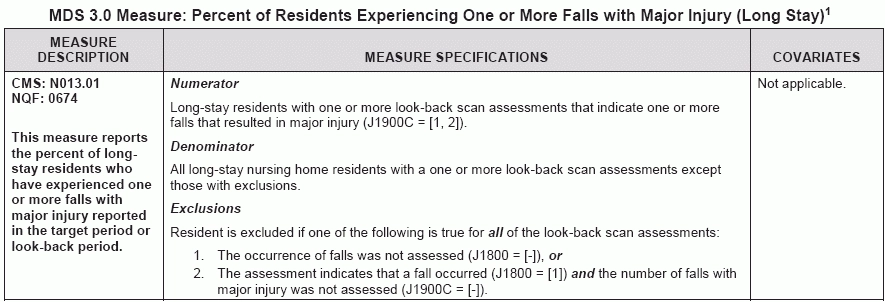
And the new QM “Percent of Residents Experiencing One or More Falls with Major Injury (Long Stay)” is triggered by just one item on the MDS: J1900 — Number of Falls Since Admission/Entry or Reentry or Prior Assessment (OBRA or Scheduled PPS), whichever is more recent. Accurate coding of J1900 is more important than ever, especially now that it can seriously impact your reimbursement.
First Step: Improve Your J1900 Coding Accuracy
“As far as the definition of a major fall, it really is clearly defined by CMS so the coding on the MDS must be accurate,” Belt says. First, you need to make certain that you look at the correct assessments. As the RAI Manual’s instructions indicate, you need to accurately code in J1900 for the OBRA (Admission, Quarterly, Annual, Significant Change Assessments) or the scheduled (five-day, 14-day, etc.) PPS assessments.
There are three types of falls and the injuries defined in the RAI Manual:
When coding item J1900, you need to go back in the medical record to admission, reentry, or since the prior assessment (which could be a period of 92 days) and determine how many falls the resident experienced, Belt instructs. Using the coding conventions above, indicate how many falls of each type of injury the resident sustained.
Stick with the RAI Manual Instructions
Also, the October 2016 updates to the RAI Manual “made it quite clear how and when to code injuries even if the information is not available until after the Assessment Reference Date (ARD) for the selected assessment,” Belt says.
Page J-32 of the RAI Manual states: “Review any follow-up medical information received pertaining to the fall, even if this information is received after the ARD (e.g., emergency room x-ray, MRI, CT scan results), and ensure that this information is used to code the assessment.”
There are occasions when the resident falls and you send him to the ER where the x-rays taken at the hospital indicate the fracture, Belt notes. And for J1900, you need to code that fracture as a major injury.
The RAI Manual also states: “If the level of injury directly related to a fall that occurred during the look-back period is identified after the ARD and is at a different injury level than what was originally coded on an assessment that was submitted to QIES ASAP, the assessment must be modified to update the level of injury that occurred with that fall.”
Prepare Yourself for the ‘Look-Back Scan’
To complicate matters even more, the falls QM uses a risk adjustment called a “look-back scan,” Belt notes. This means that once you’ve coded the MDS, CMS going forward uses a process of going back through the completed and submitted MDS records and determines if that major fall has been coded on any assessment in the last 275 days (at least).
If a long-stay resident experiences one or more falls with a major injury that you reported on one or more look-back scan assessments, this will trigger the QM, explains Kris Mastrangelo, President and CEO of Harmony Healthcare International headquartered in Topsfield, Mass. This essentially means that falls with major injury will trigger for any fall with major injury that occurred anytime during a one-year period.
Simply put, a resident will trigger this QM on your MDS 3.0 Facility QM Report if one or more of the resident’s look-back scan assessments have J1900C coded as 1 — One or 2 — Two or more, Mastrangelo says. And this QM completes a look-back scan of all eligible assessments from the five-day to the discharge assessment.
Translation: “The major fall data does not go away quickly,” Belt cautions.
Nail Down the QM Calculation
To determine the percentage calculation of the falls QM, you would identify the number of residents who experienced one or more falls that resulted in a major injury (J1900C). This is the numerator. Then, you would divide this number by the number of residents with at least two assessments in the system (the denominator).
The numerator divided by the denominator results in the percentage of long-stay residents with a major fall, Belt explains. “This is the QM that impacts the Five-Star rating and appears on the Nursing Home Comparewebsite.”
Caveat: The falls measure does have certain exclusions, Mastrangelo points out. The resident is excluded from the QM calculation if one of the following is true for all of the look-back scan assessments:
The falls QM is the same measure required under the IMPACT Act of 2014, which mandated that CMS develop and implement QMs for SNFs in the continuing effort to improve quality across the post-acute care settings, Belt points out. Although this is essentially the same QM, the one under the IMPACT Act applies only to Medicare Part A beneficiaries.
Key takeaway: If your SNF fails to comply with the data reporting requirements under the IMPACT Act, your facility faces a 2-percent reduction of its Medicare payments right off the top, Belt warns. And the QM applies to that same troublesome MDS item J1900, “so coding accuracy applies to all residents in the nursing facility. This IS major!”