Test Your Continence Coding Know-How With This Pop Quiz
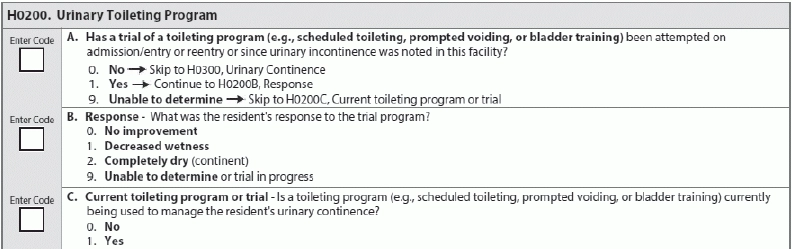
When should you code ‘unable to determine’ for H0200? Brush up on your Section H — Bladder and Bowel coding skills with a short test, based on examples in RAI Manual. Are you getting the answers to these continence items correct? After you take this quiz, turn to page 24 to see the answers. Question 1: Mrs. Smith has a diagnosis of advanced Alzheimer’s disease and is dependent on the staff for her Activities of Daily Living (ADLs). She doesn’t have the cognitive ability to void in the toilet or other appropriate receptacle and is totally incontinent. Her voiding assessment/diary indicates no pattern to her incontinence. Mrs. Smith’s care plan states that due to her total incontinence, staff should follow your facility’s standard incontinence policy, which is to check and change every two hours while awake and apply a superabsorbent brief at bedtime so as not to disturb her sleep. How should you code item H0200A — Has a trial of a toileting program (e.g., scheduling toileting, prompted voiding, or bladder training) been attempted on admission/entry or reentry or since urinary incontinence was noted in this facility? Question 2: Mr. Jones has a diagnosis of congestive heart failure (CHF) and a history of left-sided hemiplegia from a previous stroke. He has recently had an increase in urinary incontinence. The interdisciplinary team (IDT) has assessed Mr. Jones for a potential reversible cause of the incontinence and has evaluated his voiding pattern using a voiding assessment/diary. After completing the assessment, the IDT determined that Mr. Jones’ incontinence episodes could be reduced. The IDT developed and implemented a plan calling for toileting every hour for four hours after receiving his 8:00am diuretic, and then every three hours until bedtime at 9:00pm. The IDT will reevaluate Mr. Jones’ response to the care plan after one month and adjust as needed. Based on Mr. Jones’ voiding assessment/diary, the IDT determined that he could benefit from a toileting program. Therefore, you would code item H0200A as 1 — Yes. – What was the resident’s response to the trial program? Also, how should you code item H0200C — Current toileting program or trial – is a toileting program (e.g., scheduled toileting, prompted voiding, or bladder training) currently being used to manage the resident’s urinary continence? Question 3: Mrs. Brown is an 86-year-old resident with longstanding stress-type incontinence for many years. When she has an upper respiratory infection and coughs, she involuntarily loses urine. But during the current seven-day look-back period, the resident has been free of respiratory symptoms and has not had an episode of incontinence. How should you code item H0300? Question 4: Mr. Fletcher has Parkinson’s disease and is severely immobile. Staff cannot transfer him to a toilet and he is unable to use a urinal. He uses adult briefs and bed pads that staff change regularly. Mr. Fletcher did not have a continent void during the seven-day look-back period. How should you code item H0300? Question 5: Mrs. Morgan had one continent urinary void during the seven-day look-back period, after the nursing assistant helped her to the toilet and helped with her clothing. All of Mrs. Morgan’s other voids were incontinent. How should you code item H0300? Question 6: Mr. Graham has multi-infarct dementia and was incontinent of urine on three occasions on the first day of observation. He was continent of urine in response to toileting on the second and third days, and then has one urinary incontinence episode during each of the nights on days four, five, six, and seven of the look-back period. How should you code item H0300?