Don't Overlook Important Non-Section GG RAI Manual Updates
Heads up: CMS tweaked the definition of ‘Present on Admission’
If you’ve been working hard at mastering coding of the items in the new Section GG — Functional Abilities and Goals, that’s great. But you’re making a big mistake if that’s all you’re focusing on. After all, Section GG wasn’t the only significant change in the latest RAI Manual overhaul.
Here’s what you need to know about the other big revisions to the October 2016 RAI Manual v1.14:
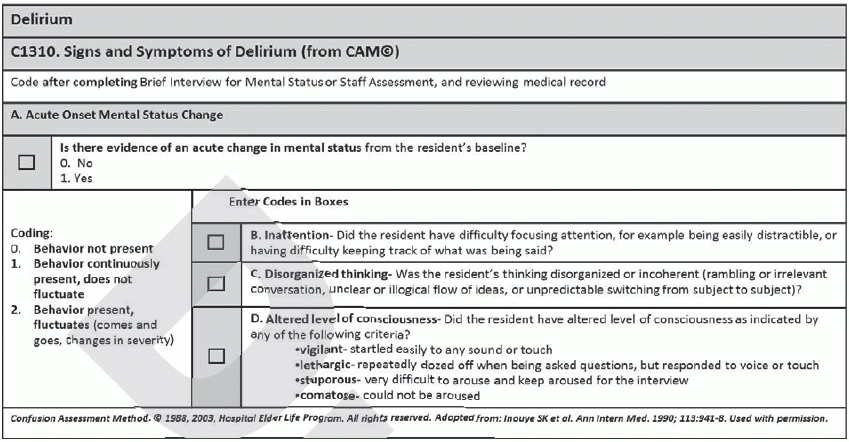
Pay Attention to CAA Effects of New Item C1310
In Section C — Cognitive Patterns and Section E — Behavior, the Centers for Medicare & Medicaid Services (CMS) removed Psychomotor Retardation, notes shelly nanney, Rn, RaC-Ct, MDS Clinical Coordinator for the Texas Department of aging and Disability services. This should help with the need to address Delirium with each Care Area Assessment (CAA), triggered by the Delirium Care Area Trigger (CAT).
Using the questions in the new item C1310 — Signs and Symptoms of Delirium, the technical component will trigger this CAA differently than in the past, Nanney says. This should cause the Delirium CAA to trigger less frequently because a worsening Brief Interview for Mental Status (BIMS) score will no longer be a triggering item.
These changes aren’t show stoppers, “but providers should make certain that the assessors coding those items understand the critical nature of accurately coding so that the possible problem of delirium is effectively captured,” notes Jane Belt, Ms, Rn, RaC-Mt, QCP, Curriculum Development Specialist for the American Association of Nurse Assessment Coordination (AANAC).
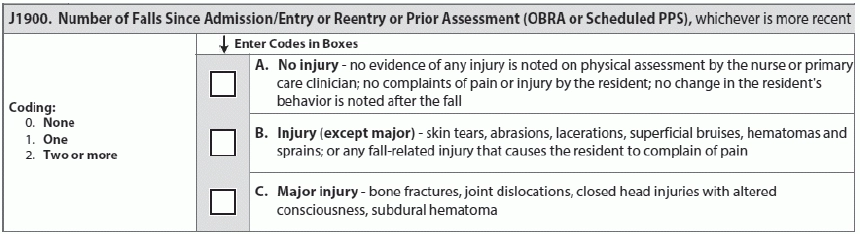
Keep Falls on Your Radar
In Section J — Health Conditions, item J1900 — Number of Falls Since Admission/Entry or Reentry or Prior Assessment (OBRA or Scheduled PPS) will play a significant role, thanks to the new falls quality measure. And now if you submit an assessment to QIES ASAP that indicates a resident had a fall but without major injury, that’s not the end of the story.
If you find out afterwards that the resident suffered a fracture, joint dislocation, altered level of consciousness, closed head injury, or other type of major injury, you will need to modify the submitted assessment to reflect the major injury, Nanney notes.
You must review any follow-up medical information such as the emergency room notes, and MRI and CT scan results, “and record those results on the MDS, even if the injuries were identified after the ARD of the MDS or after the MDS had already been submitted and accepted into QIES ASAP,” Belt explains.
Example: Mrs. Smith falls at your facility. On initial evaluation, she complains of only minor pain and doesn’t have any noticeable signs of a dislocation or fracture. Still, you send her to the hospital for evaluation, where she is admitted for dehydration and a urinary tract infection (UTI).
You complete the OBRA Discharge Assessment, coding “Discharge Return Anticipated” and J1900B — Injury (except major). Three days later, you find out that Mrs. Smith actually had a hairline fracture of her left hip.
In this case, you must modify the Discharge Assessment and code item J1900C — Major injury accordingly, Nanney explains.
Understand Clarified ‘Present on Admission’
The only changes to Section M — Skin Conditions were more clarifications to the meaning of “Present on Admission,” says terry Raser, Rn, RaC-Ct, Senior Consultant with LW Consulting Inc. For this section, you need to report three important pieces of information: 1) the history of the pressure ulcer; 2) the location; and 3) the stage on admission or reentry.
Problem: MDS accuracy audits have discovered that facilities often have conflicting documentation regarding the stage of the pressure ulcer on admission/reentry, Raser points out. When CMS conducted the pilot MDS-Focused Survey in 2014, surveyors cited 24 out of 25 pilot facilities for inaccurate coding practices.
“During the pilot, Section M (pressure ulcers) was one of the top deficient areas at 18 percent, mainly due to inconsistencies in documentation,” Raser warns. “A pressure ulcer not identified or staged in the facility’s admission documentation could be considered facility-acquired.”
All the more reason to pay close attention to the clarifications for “Present on Admission.” According to Raser, you should NOT code a pressure ulcer as Present on Admission when:
Conversely, Raser says you should code Present on Admission when:
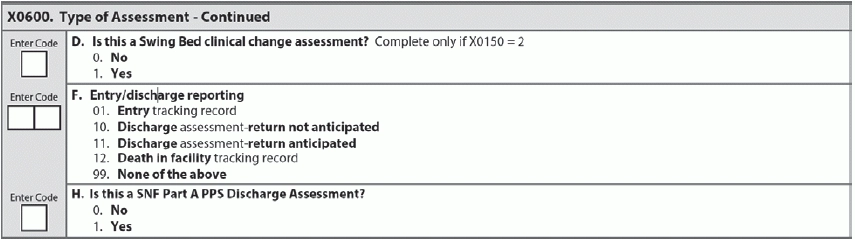
When to Code New Item X0600H
In conjunction with the new Part A Prospective Payment System (PPS) Discharge Assessment, or NPE Item Set (see “Know When You Must Complete The NPE Discharge Assessment on front page”), the RAI Manual update also added the new item X0600H — Is this a SNF Part A PPS Discharge Assessment?
CMS added this new item to facilitate modifications and in-activations to the NPE, the Polaris Group explained in a recent tutorial (www.polaris-group.com/pulse/Pulse_9_6_2016 SA.PDF). If item A0310H was incorrect on an assessment that you previously submitted and was accepted by the Quality Improvement and Evaluation System (QIES) Assessment Submission and Processing (ASAP) system, then you must modify the original assessment or inactivate it, according to the instructions in Chapter 5, section 5.7 of the RAI Manual.
Don’t Ignore 2 Minor Revisions
Finally, the latest RAI Manual update contained two other notable revisions. In Section F — Preferences for Customary Routine and Activities, CMS simply clarified that you should conduct the interview for daily and activity preferences during the observation period.
And in Section N — Medications, CMS revised the coding instructions to read that you should code N0410A-G — Medications Received “according to the pharmacological classification, not how they are being used.”
Takeaway: “Much attention has been directed to the new PPS Discharge Assessment and Section GG (they are critically important), but the accuracy of the rest of the MDS remains vital to the success of the facility as well,” Belt stresses. “The MDS drives everything we do in long-term care: surveys, reimbursement, quality measures, quality initiatives, Five-Star Ratings, and developing the on-target care plan so that the facility provides the care and services to all residents to help them achieve their highest level of function.”