What Do You Think?
Question 1: Do I need to complete Section GG for residents who were admitted before Oct. 1, 2016?
Answer 1: Yes, you must complete Section GG — Functional Abilities and Goals for residents who were admitted prior to Oct. 1 in certain situations, says Sally Fecto of Harmony Healthcare International. You should complete the Section GG items if the five-day Assessment Reference Date (ARD) is Oct. 1 or later, and/or if the Discharge or the End of Medicare Stay ARD is Oct. 1 or later.
If your MDS is rejected, this could be due to opening an MDS prior to the new software updates, Fecto notes. In this case, you need to correct the MDS and resubmit it.
Question 2: If we have an equal number of responses for Section GG, how should I determine “usual performance,” such as five times coded as 6 — Independent and five times coded as 5 — Setup or clean-up assistance?
Answer 2: Unfortunately, Section GG doesn’t offer you a handy “Rule of 3” like you have in Section G — Functional Status.
You must base all coded responses on direct observation, the resident’s self-reporting, family reports, and direct-care staff reports documented in the resident’s medical record during the three-day assessment period, according to the Pennsylvania Department of Health (PDH). “It is up to the assessor to ask further probing questions to discern which code is most accurate.”
Question 3: The resident, who is on Medicare Part A services, was admitted to the hospital in the evening. The 14-day assessment was due on the date of discharge. What do I do?
Answer 3: Complete the Discharge Return Assessment and include the minutes that were provided that day on the MDS, instructed the texas Department of aging and Disability services (DADS). You won’t complete the 14-day assessment because this pays for Days 15 through 30, for which the resident won’t be in your facility.
But the day of discharge is a non-billable day, and you cannot bill for a day when the resident isn’t in the building at midnight, DADS noted. You need to code on the MDS the services provided on the day of discharge, so that you can substantiate the level of care. When the resident returns, you will do a new five-day assessment and start over on your assessment types.
Question 4: On what day of the resident’s stay do I need to determine the performance discharge goals for Section GG?
Answer 4: Licensed clinicians can establish a resident’s discharge goals at the time of admission based on the five-day Prospective Payment System (PPS) assessment, as well as discussions with the resident and family, professional judgment, and the professional’s standard of practice, according to the PDH. You should establish the goals as part of the resident’s care plan and refer to the RAI Manual page GG-13.
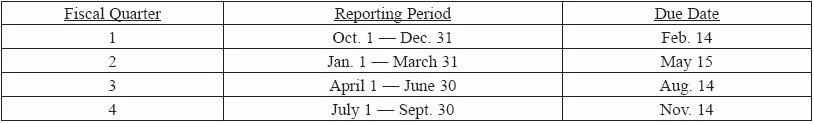
Question 5: What are the reporting period dates and deadlines for the staffing data submissions?
Answer 5: As you know, facilities must submit staffing and census information via the Payroll Based Journal (PBJ) system. The first mandatory reporting period began on July 1, 2016.
You must submit your data by the end of the 45th calendar day, by 11:59pm Eastern Standard Time, after the last day in each fiscal quarter. Therefore, the deadlines are as follows: