Improve Your A0410 Coding In 3 Steps
Warning: Don’t submit MDS records to CMS when A0410=1.
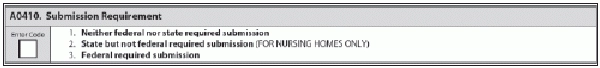
What criteria should you use to guide your coding for item A0410 — Submission Requirement? State agencies are worried that MDS coordinators don’t know the answer. Here are the steps you need to take in getting your A0410 coding right.
1. Look at A0310 Coding to Nail Down the Target Date
Your coding of A0410 hinges on the resident’s status on the target date for the assessment, according to a recent clarification memo by the Louisiana Department of Health & Hospitals (LDHH). So before you can accurately code A0410, you must first determine the target date from looking at coding in A0310 — Type of Assessment:
2. Determine Whether Resident is on a Medicare/Medicaid Unit
So based on the target date that you’ve determined, you would apply certain rules. When coding A0410, the primary question is whether the resident is in a Medicare and/or Medicaid certified unit, regardless of the payer, noted the Kansas Department for Aging and Disability Services (KDADS) in its January 2014 Sunflower Connection provider newsletter.
First, if the resident is on a Medicare/Medicaid-certified unit on the target date for the assessment, then you would code A0410 as 3 — Federal required submission, LDHH instructed.
When the unit is Medicare/Medicaid certified, you would always code 3, even if the resident is private pay or paid for through Medicare Part C (i.e., a Medicare Advantage plan or Medicare HMO), KDADS agreed.
Conversely, if the resident is on a unit that is not Medicare/Medicaid certified on the target date, you might need to code A0410 as 2 — State but not federal required submission, LDHH said. But you would code 2 only if your state requires MDS submission for individuals on the resident’s unit.
Example: Keep in mind that not all states require you to do so. For instance, Louisiana has no state only required submissions, so you would not code A0410 as 2, LDHH advised.
And if the unit is not Medicare/Medicaid certified and no state requirement exists, you would code A0410 as 1 — Neither federal nor state required submission, KDADS said.
3. Do This if Completing Assessment for Other Purposes
Finally, if you’re completing the assessment for another purpose-meaning other than to satisfy federal or state requirements-then you must also code A04210 as 1 — Neither federal nor state required submission, LDHH stated. And if you submit an MDS record in which you’ve coded A0410 as 1, the Centers for Medicare & Medicaid Services (CMS) will reject and purge the record.
Why? If you submit data that’s not required to CMS’s data systems, CMS sees this as a violation of a resident’s privacy rights, LDHH explained. Therefore, make sure you do not submit any non-required assessments to the Quality Improvement and Evaluation System (QIES) Assessment Submission and Processing (ASAP) system.
According to the RAI manual (page 5-1), nursing homes must submit Omnibus Budget Reconciliation Act (OBRA) required MDS records for all residents in Medicare- or Medicaid-certified beds, regardless of the pay source. And “skilled nursing facilities (SNFs) and hospitals with a swing bed agreement are required to transmit additional MDS assessments for all Medicare beneficiaries in a Part A stay reimbursable under the SNF Prospective Payment System (PPS).”
Also, beware that you should not transmit MDS assessments for residents who are on a Medicare Advantage plan, reminds Marilyn Mines, MDS Alert consulting editor and senior manager of clinical services for FR&R Healthcare Consulting, Inc. in Deerfield, Ill. Chapter 5-1 of the RAI manual states:
“… facilities, must transmit required MDS data records to CMS’ Quality Improvement and Evaluation System (QIES) Assessment Submission and Processing (ASAP) system. Required MDS records are those assessments and tracking records that are mandated under OBRA and SNF PPS. Assessments that are completed for purposes other than OBRA and SNF PPS reasons are not to be submitted, e.g., private insurance, including but not limited to Medicare Advantage Plans.”
Bottom line: If the reason you’re completing the assessment is not one of these reasons, you should not submit the assessment to the QIES ASAP system, “regardless of how A0410 is coded,” KDADS stressed.
Avoid Yet Another Submission Blunder
In addition to erroneously submitting MDS records to CMS when A0410 equals 1, some facilities have submitted records to the state only, but not to CMS, according to a recent issue of the California Department of Public Health’s (CDPH’s) CA MDS Nuggets provider newsletter. This happened when the MDS record indicated that A0410 equaled 3, meaning there was a federal-required submission.
“When a facility is 100-percent certified for Medicare/Medicaid, the facility is required to do a discharge assessment and the Assessment Reference Date (ARD) item A2300 must be equal to the date of discharge, A2000,” CDPH stated.
“Nursing homes must be certain to submit MDS assessments under the appropriate authority,” CDPH cautioned. The state agency also advised facilities to “have a system to make sure that transmissions are completed accurately and regularly to avoid missing assessments.”