Make Your J1100 Coding A Breath Of Fresh Air
Beware that sometimes you’ll need to check multiple sub-items here.
You can’t rely on just one information source to correctly code Item J1100 — Shortness of Breath (dyspnea). Instead, follow this proverbial trail of breadcrumbs to determine whether a resident is experiencing breathing problems and how to code this in J1100.
Why Correct J1100 Coding is So Important
Experiencing shortness of breath or trouble breathing can be distressing for residents, and it can cause decreased interaction, activity and quality of life, according to a recent training presentation by Shirley Boltz, RN, RAI/Education Coordinator for the Kansas Department for Aging and Disability Services (KDADS). Additionally, if a resident begins to experience shortness of breath, this is a potential indication of a change in condition.
There are many ways to find evidence of breathing trouble, including reviewing the medical record and interviewing the resident, staff and family members. But beware that residents sometimes don’t tell staff or family members about their shortness of breath, so that’s why it’s important to ask staff about any observations of breathing difficulties.
Residents will also often avoid activities that cause them shortness of breath to prevent breathing difficulties. These are all clues that will lead to accurate coding of Item J1100.
When to Code Each J1100 Sub-Item
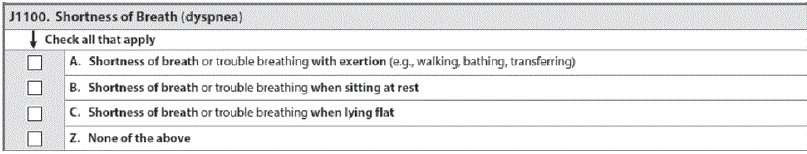
According to Boltz, Item J1100 has a seven-day look-back period and three basic coding choices to record shortness of breath or trouble breathing:
Simply put, you should check J1100A if the resident has shortness of breath or trouble breathing when he is engaging in activity, according to the Oklahoma State Department of Health (OSDH) Quality Improvement & Evaluation Service.
And keep in mind that this could be any type of activity — shortness of breath could be present during an activity as limited as turning or moving in bed during daily care, or with more strenuous activity such as transferring, walking, or bathing, the OSDH said. “If the resident avoids activity or is unable to engage in activity because of shortness of breath, then code this as present.”
Conversely, you should check J1100B if the resident experiences shortness of breath or trouble breathing when he is sitting at rest.
Check J1100C when the resident has problems breathing when he attempts to lie flat, OSDH instructed. “Also code this as present if the resident avoids lying flat because of shortness of breath.”
Finally, if the resident reports no shortness of breath or trouble breathing, and the medical record and staff interviews indicate that shortness of breath appears to be absent or well controlled with current medication, check J1100Z — None of the above, OSDH said.
Check All that Apply
In many cases, the resident may experience shortness of breath or trouble breathing in more than one of the scenarios described in Item J1100. The OSDH provides the following example:
Scenario: Mrs. W. has a diagnosis of chronic obstructive pulmonary disease (COPD) and heart failure. She is on two liters of oxygen and daily respiratory treatments. With oxygen, she is able to ambulate and participate in most group activities, but she reports feeling “winded” when walking the length of the hallway or going to the dining room.
Staff have observed Mrs. W. having to stop and rest several times, and recently, she describes feeling “out of breath” when she tries to lie down.
How to code: Because Mrs. W. reported being short of breath when lying down, as well as during walking that required ambulating longer distances, you would check both J1100A and J1100C.