What Do You Think?
Question 1: What’s the proper way to document respite care in the MDS 3.0?
Answer 1: “Respite refers to short-term, temporary care provided to a resident to allow family members to take a break from the daily routine of caregiving,” explains the Oklahoma State Department of Health (OSDH) Quality Improvement & Evaluation Service. For all respite residents, you must complete an Entry tracking record and a Discharge assessment.
If the respite stay is 14 days or longer, you must complete an Omnibus Reconciliation Act of 1987 (OBRA) Admission assessment, OSDH instructs. Also, you must complete the care plan seven days after you complete the admission assessment (RAI Manual, page 2-14). And don’t forget to initiate an interim care plan to guide staff in resident care if the admission OBRA assessment is not yet completed.
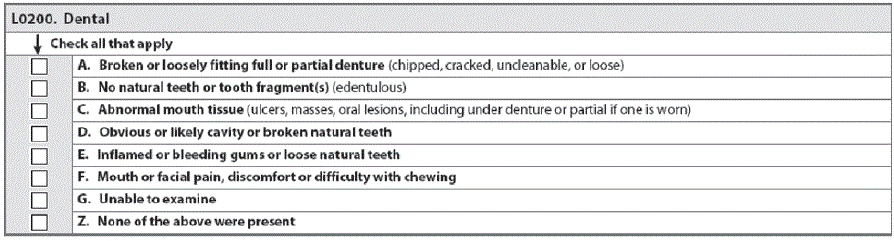
Question 2: When a resident has dentures or a partial, do I need to check L0200B?
Answer 2: You should check L0200B — No natural tooth or tooth fragment(s) (edentulous) if the resident is edentulous or lacks all natural or parts of teeth, said Carol Siem, MSN, RN, GNP-BC, RAC-CT, Educator and Team Leader for the Quality Improvement Program for Missouri’s Long-Term Care Facilities (QIPMO).
L0200B is not asking if the resident has dentures, which is addressed in the previous question, L0200A — Broken or loosely fitting full or partial denture (chipped, cracked, uncleanable, or loose), Siem noted. Instead, L0200B is asking if the resident has any teeth at all.
Question 3: Some quality measures (QMs) on our report cite items that occurred a long time ago, including some that happened when the resident wasn’t even in our facility. Are these mistakes?
Answer 3: “Some Long Stay measures utilize MDS items that record events or conditions that occurred since the prior assessment was performed,” the OSDH explains. “The purpose of the look-back scan is to determine whether such events or conditions occurred during the look-back period.”
These QMs will trigger if the event or condition in question occurred any time during a one-year period — the exact time period used is 275 days, to include up to three quarterly OBRA assessments. The Centers for Medicare & Medicaid Services (CMS) examines all assessments with target dates in this time period to determine whether the event or condition of interest occurred at any time during the period.
What’s more: Also, due to this look-back period, you may see items listed on your report that occurred while the resident was not in your facility and before you admitted the resident, according to the OSDH. You can find more information on why some QMs remain on your report this long in the QM User’s Manual, Chapter 1, page 7.
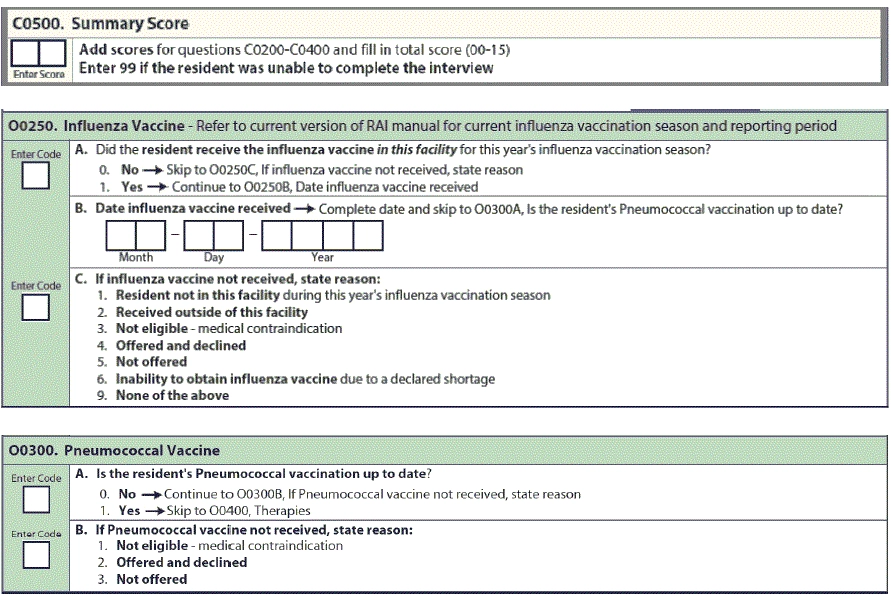
Question 4: Should we chart a care-plan intervention of reminding the resident to use the call light if that resident scored less than 13 on the Brief Interview for Mental Status (BIMS)?
Answer 4: No, if the resident’s BIMS score that you record in Item C0500 — Summary Score is less than 13 (“cognitively intact” is a score of 13 to 15), a care plan intervention of reminding the resident to use the call light “is not going to be very effective,” Siem stated. This is also a common mistake when a resident’s baseline memory is already poor.
Remember: The items in Section C — Cognitive Patterns are intended to determine the resident’s attention, orientation, and ability to register and recall new information, Siem stressed. “These items are crucial factors in many care planning decisions.”
Question 5: With two versions of the pneumococcal vaccine available, how should we code each one specifically in the MDS?
Answer 5: CMS has not yet updated Item O0300 — Pneumococcal Vaccine to reflect the availability of two versions of the pneumococcal vaccine, Siem noted. Until CMS updates this item, simply code O0300A — Is the resident’s Pneumococcal vaccination up to date? as 1 — Yes, if the resident has received either vaccine or both.
And now that we are in the midst of flu season, you should pay close attention to your coding of Item O0250 — Influenza Vaccine. Remember that once you document the flu vaccine in Item O0250, you should continue to code it on every MDS that you complete for the resident until the next flu vaccination season begins — which is typically when your facility receives the new batch of flu vaccine, according to the Texas Department of Aging and Disability Services (DADS).
Also, keep in mind that if the MDS is due before you give the flu vaccine, you should code O0250C — If influenza vaccine not received, state reason as 5 — Not offered, Siem instructed. CMS does not calculate your vaccination rates for Nursing Home Compare until the end of the season, so by the time you complete the next MDS you will be able to update on the new MDS that the resident received the vaccine.