Improve Your O0300 Coding With These Expert Tips
Coding doesn’t exclude different types of pneumococcal vaccine.
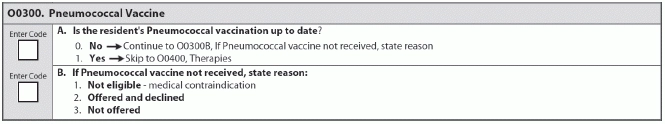
Do you know the “who,” “what,” “where,” and “how often” factors regarding pneumonia vaccinations? If not, you’re probably coding Item O0300 — Pneumococcal Vaccine the wrong way. Here’s what you need to know.
Who Should Receive the Vaccine?
According to the RAI manual, all residents over the age of 65 and immunocompromised persons two years of age and older should receive the pneumococcal vaccine. Also, individuals living in nursing homes, other long-term care facilities, or other environments or social settings “with an identified increased risk of invasive pneumococcal disease or its complications” should receive the vaccine.
And pneumonia is a particularly serious concern for your elderly residents. According to Centers for Disease Control and Prevention (CDC) statistics, case fatality rates for pneumococcal bacterial infection can be as high as 60 percent in elderly individuals, warned the Texas Department of Aging and Disability Services (DADS) in its December 2014 MDS Mentor.
How Often Should Your Administer?
The pneumococcal vaccine is once in a lifetime, except in certain situations, independent consultant Jennifer Pettis, BS, RN, WCC said in a recent presentation for the Wyoming Department of Health’s Aging Division. Individuals who may need the pneumococcal vaccine more than once in their lifetime include:
Where You Should Look for Necessary Info
According to Pettis, you should also take the following steps for assessing Item O0300:
1. Review the medical record: First, look at the resident’s medical record to determine whether he’s received a pneumococcal vaccine. If the resident’s status is unknown, go on to the next step.
2. Ask around: Ask the resident, his family and his primary care physician whether the resident has received the pneumococcal vaccine. If the resident’s status is still unknown, go to the next step.
3. Vaccinate: If you cannot determine whether the resident has received the pneumococcal vaccine, vaccinate the resident as appropriate according to the standards for vaccination.
Tip: Another place to look is in the Common Working File (CWF) or HIPAA Eligibility Transaction System (HETS), suggests Marilyn Mines, RN, BC, RAC-CT, MDS Alert consulting editor and senior manager of clinical services for FR&R Healthcare Consulting Inc. in Deerfield, Ill. “If the resident has Medicare Part B, more likely than not whoever administered the vaccination billed the Medicare program.” You will then see the date the vaccination was billed on the “prevention” screen of the system you’re using.
What Type of Pneumo Vaccine Doesn’t Matter for Coding
Another consideration is which pneumococcal vaccine to administer. The PCV7 vaccine protects against seven different bacteria that cause pneumonia, while the PCV13 vaccine protects against 13 types, DADS noted.
Both the PCV7 and PCV13 are valid types of the pneumococcal vaccines, however, and you can code the use of either one on the MDS in Item O0300, DADS said.
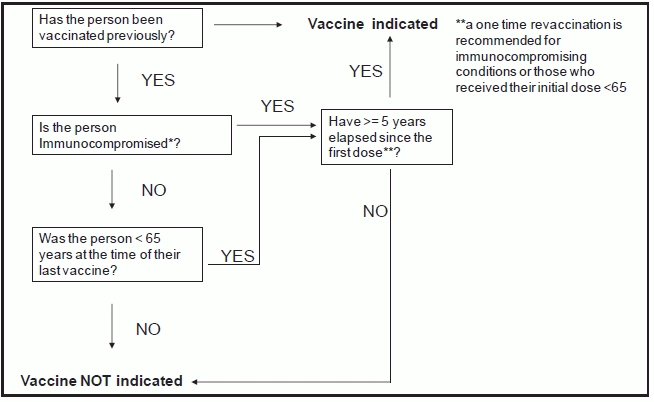
Use This Algorithm to Decide Whether to Vaccinate
The RAI manual also includes a helpful algorithm on page O-12 that can assist you in deciding whether you need to administer the pneumococcal vaccine to a resident. CMS adopted the algorithm from the CDC Advisory Committee on Immunization Practices’ recommended adult immunization schedule.