Here's How Lesion Type/Size and Layer Closer Can Validate Your Vulvar Lesion Claims
Here’s How Lesion Type/Size and Layer Closer Can Validate Your Vulvar Lesion Claims
Avoid the costly mistake of using an integumentary code instead of a vulvectomy one.
In order to correctly choose between a vulvectomy versus a vulvar lesion excision code, your ob-gyn must document the type of lesion, lesion size (plus margin), and the layer closure.
Check your relative value units (RVUs). All vulvectomies have more RVUs than lesion excisions because vulvectomies involve much more work, says Melanie Witt, RN, CPC, COBGC, MA, an independent coding consultant in Guadalupita, N.M. For instance, 56620 (Vulvectomy simple; partial) pays $533.97 while the most expensive of malignant lesion excision codes (11620-11626, Excision, malignant lesion including margins, scalp, neck, hands, feet, genitalia …) carries a $415.75 facility allowable. That’s a difference of $118.22.
Choose Vulvectomy For Non-Discrete, Large Tissue Areas
If the lesion is not discrete and involves large areas of tissue (such as extensive dysplasia), your ob-gyn will perform a vulvectomy:
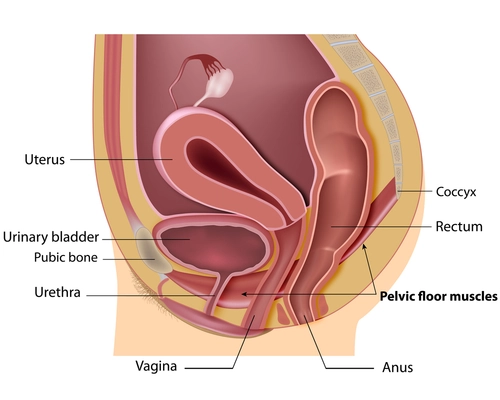
Definition: CPT® defines a simple vulvectomy as the removal of skin and superficial subcutaneous tissue. The classic definition of a simple vulvectomy is the removal of benign disease by the superficial removal of vulvar structures (such as labia minora, labia majora, clitoris, etc.), including the skin, mucous membrane, and any superficial fat and connective tissue, Witt says.
Key terms: When reporting a vulvectomy, you should watch for key terms. For instance, a radical vulvectomy, includes excising the skin and deep subcutaneous tissue. A partial vulvectomy means the physician removes less than 80 percent of the vulva (for example, the left labia).
Focus on Lesion Size for Integumentary Codes
For lesions that are discrete and localized, however, you will look at the “Integumentary System” chapter of your CPT® book — and not the “Female Genital System” chapter.
Benign: You should report 11420-11426 (Excision, benign lesion including margins, except skin tag [unless listed elsewhere], scalp, neck, hands, feet, genitalia …) for the excision of discrete vulvar lesions, which require removal of only narrow surgical margins. What code you report depends on the lesion’s size — plus the margin removed.
Malignant lesions usually involve wide excisions. For this, you should report 11620-11626 (Excision, malignant lesion including margins, scalp, neck, hands, feet, genitalia …). Again, what code you report depends on the lesion’s size plus any margins. In some cases, when the ob-gyn cannot confirm a lesion as benign, but the ob-gyn still takes wide margins while removing the lesion, you still may report the malignant excision codes.
You May Be Able to Report Layer Closure
If your ob-gyn has to do more than a simple closure of the remaining tissues (an intermediate or complex repair), you should add another code. You may report 12041-12047 (Layer closure of wounds of neck, hands, feet and/or external genitalia …) or 13131-13133 (Repair, complex, forehead, cheeks, chin, mouth, neck, axillae, genitalia, hands and/or feet …).
Watch out: The size of the lesion and that of the repair must match your ob-gyn’s documentation. Also, if a complex repair is 1.0 cm or less, CPT® instructs you to report the repair as intermediate, not complex, Witt says.
Don’t Overlook Dx
Along with scrutinizing your ob-gyn’s documentation for lesion size, lesion margin, and layer closure, you should take note of the patient’s diagnosis. For instance, an infection (such as the human papilloma virus [HPV]) or irritant may cause vulva dystrophy.
ICD-10-CM offers the following codes:
Did you know? If the pathology report returns with indications of dysplasia, the neoplasm is in transition from being benign to becoming malignant. If the process continues and the mass is left untreated, the neoplasm could eventually become malignant, Witt points out.