New Myomectomy Codes Require Complete Documentation to Ensure Proper Payment
Reviewed on May 20, 2015
The number and weight of excised myomas are the keys to reporting the new myomectomy codes introduced in CPT® 2003. Consequently, if your physician doesn't record this information, you may be forced to report lower codes, which will cut into your ob-gyn practice's bottom line.
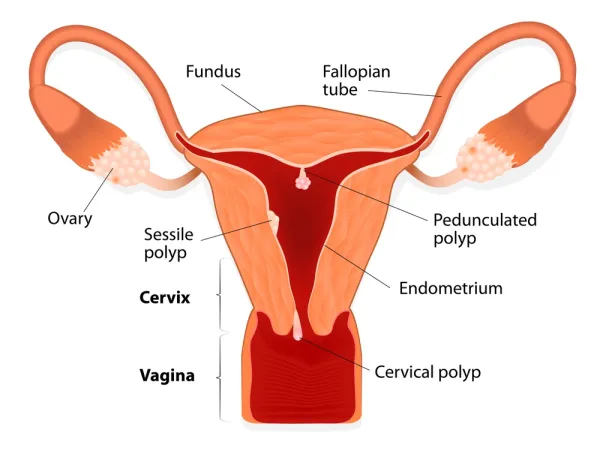
Ob-gyns perform myomectomies to surgically remove uterine fibroids (218.x), or myomas. The physician can take out the myomas either endoscopically, with a vaginal approach, or with an open procedure.
Use 58140 for Open Abdominal Approach, but 58145 for Vaginal Approach.
CPT® includes five codes for myomectomies. Three are new, and one is revised for 2003. The revised code, 58140 (Myomectomy, excision of fibroid tumor[s] of uterus, 1 to 4 intramural myoma[s] with total weight of 250 grams or less and/or removal of surface myomas; abdominal approach), previously did not specify the number or weight of the myomas, but only that the ob-gyn performed the procedure as an open abdominal approach. It now specifies one to four intramural myomas with a total weight of 250 grams. If the surgeon removes the myomas vaginally, you should use 58145 (…vaginal approach).
You also should use these codes when the physician removes surface myomas. CPT® does not designate a particular number of surface myomas necessary for billing 58140 or 58145. This may be because "surface myomas do not take a whole lot of time, even if there are a whole bunch of them," says Melanie Witt, RN, CPC, MA, an ob-gyn coding expert.
Coding Example: A 35-year-old woman reported to her ob-gyn for abnormal uterine bleeding. Although the physician has tried medications and dilation and curettage, they have not been successful in treating the condition. Using ultrasonography, the doctor finds three scattered intramural and subserosal myomata ranging in size from 1 cm to 5 cm. The ob-gyn decides to perform an open abdominal myomectomy because of the fibroids' location. In this case, you would report the myomectomy with 58140, linked with 218.1 (Intramural leiomyoma of uterus) and 218.2 (Subserous leiomyoma of uterus).
In ICD-10, you will use D25.1 (Intramural leiomyoma of uterus) and D25.2 (Subserous leiomyoma of uterus) instead.
New Code 58146 Represents Multiple/Large Myomas
Code 58146 (Myomectomy, excision of fibroid tumor[s] of uterus, 5 or more intramural myomas and/or intramural myomas with total weight greater than 250 grams, abdominal approach) is brand new for 2003. You should use this code when the ob-gyn excises five or more uterine fibroid tumors. But remember that the documentation must state that they are intramural myomas. You also can bill this code if there are only one to four intramural myomas, but their total weight must be greater than 250 grams. As with 58140, 58146 represents an open abdominal approach, and you should link the code to the diagnosis for intramural leiomyoma (218.1).
Coding Example: The ob-gyn sees a 32-year-old patient who has never had a child, but would like to. She complains of heavy menses with anemia. On examination, the physician finds a 15-cm uterus with multiple fibroids that distort the endometrium. Because the patient wishes to have children, she elects to have a myomectomy, which the ob-gyn performs using an abdominal approach. The pathology report shows six intramural myomas. For this case, you should report 58146 with 218.1.
"There is no vaginal approach procedure code for the larger-size fibroid because generally they are so large it's almost impossible to get them out by that route," Witt explains. "At least, that was the thinking when they changed the codes."
Tip: Because submucous myomas (218.0) are located inside the uterine cavity, physicians normally remove them through a hysteroscope (58561). You should note that this code does not specify any required weight or number of myomas.
Report 58545 and 58546 for Laparoscopic Procedures
The two remaining new myomectomy codes for 2003 are 58545 (Laparoscopy, surgical, myomectomy, excision; 1 to 4 intramural myomas with total weight of 250 grams or less and/or removal of surface myomas) and 58546 ( 5 or more intramural myomas and/or intramural myomas with total weight greater than 250 grams). These codes represent the laparoscopic alternative to the open procedures shown in 58140 and 58146. Because CPT® distinguishes between these laparoscopic codes by the number of fibroids and their weight, these will be key components of the ob-gyn's documentation.
Coding Example: A 34-year-old patient who recently married and is anxious to have children complains to her ob-gyn of heavy menstruation that is causing her to feel fatigued. After examining the patient, the doctor finds a 13-cm uterus that contains four fibroid tumors. He performs a laparoscopic myomectomy to remove the myomas. Here, you would report 58545 if the total weight of the four myomas is less than or equal to 250 grams. Diagnostically, you would want to wait for the pathology report to ensure that you link the correct diagnosis code to the procedure.
If you bill prior to knowing the type of myoma, the only code you can report is 218.9 (Unspecified leiomyoma of uterus). For some payers, an unspecified code after surgery may lead to a claim denial.
In ICD-10, you will report D25.9 (Unspecified leiomyoma of uterus) instead.
Count and Weigh Your Fibroids
The key to using these codes is that physician documentation must change. You now have to select the proper code based on the number and weight of the fibroids. The ob-gyn also must indicate whether he or she used an abdominal approach laparoscopic or a vaginal approach.
The extra burden of weighing the myomas is well worth it. "My opinion on the new codes is that it causes more work for the physicians and/or the coders," says Maureen Murphy, CPC, a coding specialist at Mount Kisco Medical Group in Mount Kisco, N.Y. "But if the physician does the extra work, why not get the reimbursement for it?" she suggests.
"This may sound funny, but if a physician wants to get this as part of his documentation early, he really needs to have a scale in the operating room, or you can wait for the pathology report," Witt says. "If you do not want to or the physician says I am not going to bother with that and you do not find the documentation of the number or the weight, you must default to those lower codes, the 58140 and 58545."
Getting the weight does make a difference, Murphy emphasizes.