Time Alone Is Sufficient to Select a Counseling Level of Care

Watching the clock can make all the difference.
Many factors go into selecting an E/M code, but CPT® considers time to be the key to determining the appropriate code for provider/patient counseling. Here’s your refresher on how to arrive at the correct code for these situations.
Remember What’s Included
When you code based on time for professional fee services in the outpatient setting, you can count only the face-to-face time with the patient or family. This time calculation includes the time spent counseling as well as the time associated with any history, exam, or medical decision making. The time spent reviewing records, talking with other providers, and documenting the encounter without the patient or family present cannot be considered part of counseling time.
Starting point: CPT® states, “When counseling and/or coordination of care dominates (more than 50%) the physician/patient and/or family encounter (face-to-face time in the office or other outpatient setting or floor/unit time in the hospital or nursing facility), then time may be considered the key or controlling factor to qualify for a particular level of E/M services.” When the most of the encounter involves counseling or coordination of care, time – not the extent of history, exam, or medical decision making – is the key to determining the correct code.
For E/M services, counseling may include:
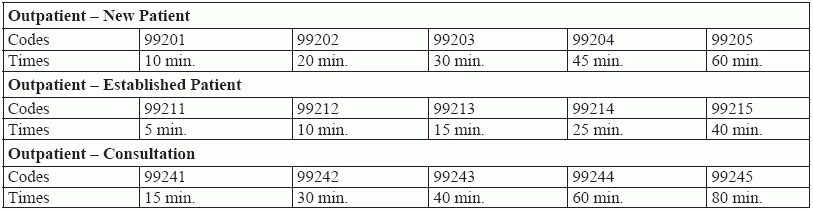
The time reference is stated in the final sentence of the E/M code descriptor. For instance, consider the descriptor for new patient outpatient service 99203: Office or other outpatient visit for the evaluation and management of a new patient, which requires these 3 key components: A detailed history; a detailed examination; Medical decision making of low complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the presenting problem(s) are of moderate severity. Physicians typically spend 30 minutes face-to-face with the patient and/or family.
Note that the descriptor specifies, “Physicians typically spend 30 minutes face-to-face with the patient and/or family.” In contrast, according to CPT® guidelines, “Time is not a descriptive component for the emergency department levels of E/M services because emergency department services are typically provided on a variable intensity bases.” Likewise, observation codes 99234-99236 do not have a time reference. Because these services do not include time references, you should not report them with time as the controlling element.
Document the Extent of the Counseling
Statements such as “extensive discussion” or even “discussed at length” do not match to a specific CPT® code, which makes the amount of time open to interpretation. Document the actual time spent with the patient (e.g., 15 minutes) to help pinpoint the best coding options.
If the encounter involved counseling as well as time spent performing the key components of an E/M service, the best practice is to indicate the total time spent with the patient and specify that more than half of the encounter involved counseling. This verifies that the requirements for using time to select an E/M code have been met and makes it clear that time was the determining factor for the code selected.
Example: An 18-month-old child with an injured leg is brought to the office. The provider completes two out of the three key components (expanded problem focused history, expanded problem focused exam, or medical decision making of low complexity). After reviewing the patient’s chart, the physician notices that the child is due for a refill of his asthma medication. The physician inquires about the ongoing medication and its impact. The mother discusses recent issues with getting the child to cooperate taking his medications. The physician spends a great deal of time counseling the mother on ways to administer the medications and how to be sure the child is getting enough. The physician also advises the mother on the importance of taking peak flow meter ratings.
Before coding the encounter, you need to know exactly how much time the physician spent counseling the patient (through his mother). Determining that will show what percentage of the total time of the visit was spent on counseling, which in turn will point you to the correct E/M code. Take a look at the table below, to see how the codes change according the time spent on counseling.
Coding tip: You can often find clues in the schedule or the nurse’s notes that can alert you to encounters that might be appropriate for selecting your code based on time. For example, time-based coding is likely if the visit is primarily to discuss lab results or to follow up on a new medication, or if family members have accompanied the patient. For any case, the more you can encourage your providers to check their watches before and after rendering service, the better your E/M coding will be.