Master Lesion Destruction Claims with Answers to 3 Common Myths

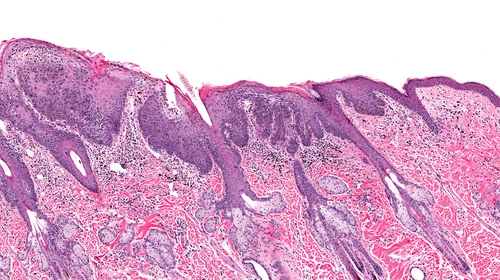
Hint: Utilize the CPT® documentation to code without error. Are you in the know when it comes to reporting destruction of skin lesions using methods like laser surgery, or cryosurgery? You need to report more than just the type of skin lesion you destroy to avoid denials. Don’t fall victim to these lesion destruction coding myths — arm yourself with the facts. Myth 1: It’s a Numbers Game Reality: While you do report some types of skin lesion destructions based on the number of lesions your clinician removes, you won’t report all skin lesion destructions in this manner. When your clinician destroys premalignant lesions or benign skin lesions using methods like laser surgery, cryosurgery, and other such means, you must select the appropriate code(s) based on the number of lesions your clinician removed. For destruction of premalignant lesions, you have three code choices to report from based on the number of lesions destroyed: And, for destruction of benign lesions, you have two code choices to report from based on number of lesions destroyed: On the other hand, if your clinician performs destruction of malignant lesions, you should focus on the anatomical location and the size of the lesion that was destroyed because these form the basis for reporting the appropriate code for the procedure. You have three code ranges to choose from based on the anatomical location and size of the lesion: Note: “The instructions in the CPT® Manual tell you exactly how to report such a service,” says Suzan (Berman) Hauptman, MPM, CPC, CEMC, CEDC, senior principal of ACE Med, a medical auditing, coding and education organization in Pittsburgh, Pennsylvania. When reporting destruction of premalignant lesions, you report the CPT® code 17000 for destruction of the first lesion and then report one unit of the add-on code for destruction of each additional lesion (when your clinician destroys up to or less than 14 lesions). “If your clinician destroys 15 or more lesions, only the code 17004 should be reported,” says Mary I. Falbo, MBA, CPC, CEO of Millennium Healthcare Consulting, Inc. in Lansdale, Pennsylvania. Similarly, when your clinician destroys benign lesions, you report CPT® code 17110 only once when your clinician destroys between one to 14 lesions. If the number of lesions your physician destroys is more than 14, you only need to report 17111 one time. “For destruction of benign lesions like common warts or flat warts, use CPT® codes 17110 or 17111 depending on the number of lesions,” Falbo says. “The documentation along with the description found within CPT® will guide you to the proper code,” Hauptman adds. Myth 2: Every Destruction Code Requires an E/M Code Reality: As with most procedural codes, you should not report an additional E/M code with destruction codes as a norm. You should report an E/M code with the destruction code if and only if the E/M service is significant and separately identifiable from the destruction. If the E/M service is significant and separately identifiable, you can report both the destruction and the E/M code. You will need to append the modifier 25 (Significant, separately identifiable evaluation and management service by the same physician or other qualified healthcare professional on the same day of the procedure or other service) to the E/M service code. “This is because E/M services are otherwise bundled into the skin lesion destruction codes as part of Correct Coding Initiative (CCI) edits,” says Kent Moore, senior strategist for physician payment at the American Academy of Family Physicians. “The CCI edits permit the bundles to be broken with an appropriate modifier, such as modifier 25.” Example: Your FP reviews a 49-year-old established male patient with type 2 diabetes for a scheduled visit to assess the patient’s blood sugar levels. During the visit, the patient also complains of a recent occurrence of multiple reddish skin eruptions on the face and arms that are slightly painful, if touched. Your physician performs an expanded problem-focused history and exam, and medical decision-making of moderate complexity related to the diabetes and notes elevated blood sugar levels. On examination of the skin lesions, your clinician diagnoses the lesions as solar keratosis and removes them by cryosurgery. In the patient notes, your clinician mentions that 12 lesions were destroyed (four on the face and eight on the arms). What to report: Your clinician performed a level three E/M service for the evaluation and management of the patient’s diabetes and performed removal of 12 premalignant lesions by cryotherapy. Your claim should include the following codes: “Remember that modifier 25 does not necessarily require a different diagnosis,” Moore notes. “Per CPT®, the E/M service may be prompted by the symptom or condition for which the procedure and/or service was provided. As such, different diagnoses are not required for reporting of the E/M services on the same date. If you have different diagnoses, such as in this example, that helps support that the E/M was significant and separately identifiable. But different diagnoses are not required if the documentation supports that the work of the E/M was over and above that which is usually associated with the procedure.” Myth 3: Premalignant, Benign, Malignant Skin Lesion Destructions Cannot be Reported Together Reality: You will hit a roadblock if you are trying to report destruction of premalignant lesions and benign lesions together. These two code sets are bundled by Correct Coding Initiative (CCI) edits. Similarly, you run into bundling edits if you try reporting destruction of premalignant lesions and malignant lesions together. However, the modifier indicator for these code bundles is ‘1,’ which means you can use a suitable modifier to unbundle the codes and report them separately. To bundle the destruction of premalignant lesions and benign lesions, the CPT® codes 17000-17004 that you report for destruction of premalignant lesions form the column 2 codes. So, you will append modifier 59 (Distinct procedural service) to the premalignant lesion destruction code you are reporting. You would also do the same for the CPT® code for the destruction of malignant lesions.