Decipher CMS’ Digital Health Decisions in the 2024 MPFS Final Rule
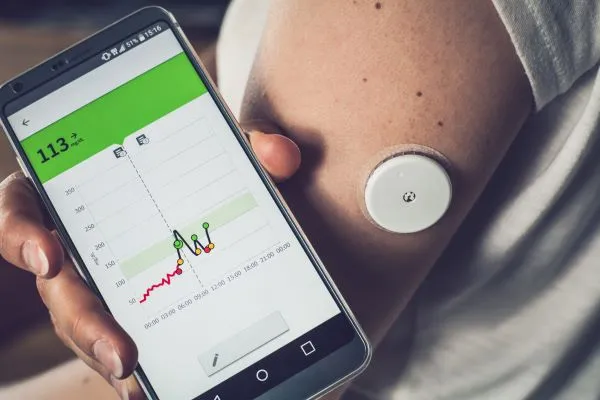
How many data transmission days are required for RPM/RTM? The Centers for Medicare & Medicaid Services (CMS) published its calendar year (CY) 2024 Medicare Physician Fee Schedule (MPFS) final rule in the Federal Register on Nov. 16, 2023. Among the 1,230 pages are rulings on telehealth and remote monitoring services. Tech & Innovation in Healthcare pored over the agency’s rule to see how it will affect your 2024 reimbursement. Check in With Post-PHE Telehealth Services Policies During the COVID-19 public health emergency (PHE), the Medicare telehealth services expansion allowed many providers to continue to care for their patients. For CY 2024, CMS continues to push forward with several finalizations. Place of service codes: Effective January 1, telehealth services that are provided in the patient’s home billed with place of service (POS) 10 (Telehealth provided in patient’s home) will receive reimbursement at the higher, non-facility MPFS rate. At the same time, services billed with POS 2 (Telehealth provided other than in patient’s home) will continue to be reimbursed at the MPFS facility rate for originating sites that are not the patient’s home. These sites can include a physician’s office or a hospital. Telehealth taxonomy: The agency finalized its proposal to add telehealth services on “permanent” or “provisional” statuses rather than the Category 1, 2, or 3 taxonomy that was in effect throughout the PHE. “In this Final Rule, CMS finalizes its proposal to simplify its multicategory approach and consider additions to the list as either permanent or provisional beginning in 2024. The process remains consistent with the existing principles applied during the COVID-19 PHE,” writes Miranda A. Franco, senior policy advisor, with law firm Holland & Knight LLP in online analysis of the final rule. Going forward, telehealth services will receive the permanent or provisional status after going through a five-step process. Policy extension: The Consolidated Appropriations Act of 2023 (CAA 2023) extended several telehealth policies through the end of 2024, and CMS noted the policies’ implementation in the final rule. The provisions include removing telehealth frequency limitations for nursing facility visits, subsequent inpatient visits, and observation stays. CMS also extended payment for audio-only telehealth evaluation and management (E/M) services through the end of 2024. These services are reported with the following codes: Additionally, CMS has finalized extending the direct supervision definition through Dec. 31, 2024. Direct supervision now includes a physician’s or other practitioner’s presence on real-time audio/video communication technology, but not audio-only visits. Recognize RPM and RTM Changes In the CY 2024 MPFS proposed rule, CMS proposed that remote physiologic monitoring (RPM) and remote therapeutic monitoring (RTM) services may be furnished only to established patients. CMS finalized half of that proposal in the final rule — the agency stated that providers must have an established relationship with the patient to provide RPM, not RTM, services. “For RTM, CMS noted that they have not specified in previous rules that RTM is limited to established patients but that they expect the billing practitioner to establish a treatment plan prior to providing RTM services,” writes Carrie Nixon, Esq, managing partner, and Kaitlyn O’Connor, Esq, partner, of Nixon-Gwilt Law in Virginia, in online analysis. No primary care: CMS received feedback from stakeholders during the comment period regarding the agency’s proposal to set 99457-99458 (Remote physiologic monitoring treatment management services, clinical staff/physician/other qualified health care professional time in a calendar month requiring interactive communication with the patient/caregiver during the month …) as primary care under the Medicare Shared Savings Program (MSSP). “Stakeholders were concerned that if RPM services were categorized as primary care, specialists and other non-[accountable care organization (ACO)] providers that provide RPM could inadvertently divert assigned beneficiaries away from ACOs, disrupting plurality and utilization calculations,” write Nixon and O’Connor. As a result of the comments, CMS finalized not classifying RPM as primary care for MSSP beneficiary assignment. Find out if Treatment Management Codes Need 16 Days of Data CMS finalized that the following treatment management codes do not require 16 days of data in a 30-day period: CMS recommended that the RPM and RTM treatment management codes listed above would require at least 16 days of data transmission over 30 days. However, this proposal was met with disagreement from stakeholders.