rfarnham91
New
Hello everyone! I really hope this is the right forum to post this question. I apologize if it isn't.
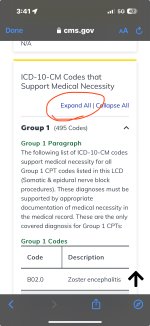
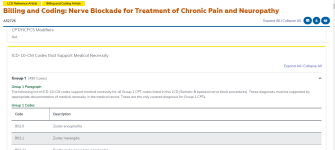
I am still relatively new when it comes to coding but I recently started a job in denials management. The job has been a great way to dip my toes in understanding insurance payor policies and CMS guidelines. There is this one claim that has me stumped. CPT 64415 was denied per CMS policies due to incorrect DX. The main dx is S42.021A and the secondary are Z88.0 and Z79.01. Normally when I look up the article in the CMS database and will have the dx code for either allowed or not. However when I looked at Billing and Coding: Nerve Blockade for Treatment of Chronic Pain and Neuropathy the cpt code is listed however not any of the dx are listed at all. I'm not sure if I am looking up the wrong article or what else I am missing. Like I said, I am still very green but I want to get to the bottom of this and learn from this as well. If there is any further information needed please ask. I kept this as vague as possible to protect patient information. Thanks!
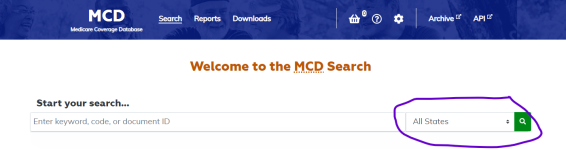
Here is the website of the article on the cms database
I am still relatively new when it comes to coding but I recently started a job in denials management. The job has been a great way to dip my toes in understanding insurance payor policies and CMS guidelines. There is this one claim that has me stumped. CPT 64415 was denied per CMS policies due to incorrect DX. The main dx is S42.021A and the secondary are Z88.0 and Z79.01. Normally when I look up the article in the CMS database and will have the dx code for either allowed or not. However when I looked at Billing and Coding: Nerve Blockade for Treatment of Chronic Pain and Neuropathy the cpt code is listed however not any of the dx are listed at all. I'm not sure if I am looking up the wrong article or what else I am missing. Like I said, I am still very green but I want to get to the bottom of this and learn from this as well. If there is any further information needed please ask. I kept this as vague as possible to protect patient information. Thanks!
Here is the website of the article on the cms database