M1040: Break Down and Code Skin Problems Beyond Pressure Ulcers
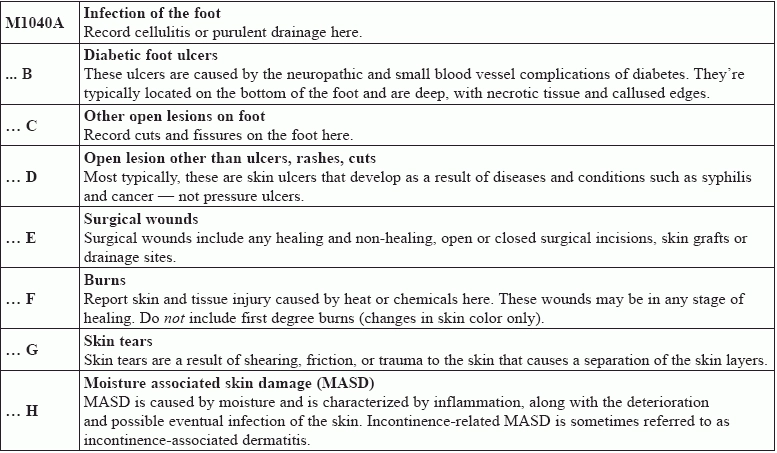
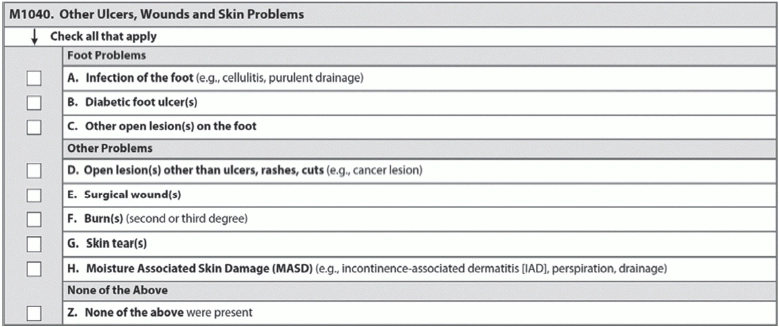
Check in on skin issues, head to foot, and learn tips to code pressure ulcers after surgical intervention. Section M isn’t all about the pressure ulcers; make sure you’re utilizing item M1040 (Other Ulcers, Wounds and Skin Problems) to document residents’ skin health. When deciding how to code item M1040, think about skin as the body’s largest system; pay careful attention to wounds or lesions that could be indicative of deeper systemic problems. Remember, too, that circulation issues common in older people can often manifest as foot problems. Item M1040 is where you document footissues, too. Skin issues can have an outsize impact on a resident’s quality of life and cause pain that might prevent him or her from participating fully in daily life. Know These Assessment Basics What qualifies as “Other ulcers, wounds and skin problems”? The RAI Manual has helpful definitions as to what’s appropriate to record. When looking over the resident’s clinical record (including skin care flow sheets and other skin tracking forms), talking to team members involved in direct care, and speaking to the resident and conducting an examination, consider these RAI Manual definitions before completing item M1040: Remember: Do not code rashes or cuts/lacerations in item M1040D (Open lesion other than ulcers, rashes, cuts). Though you won’t record them on the MDS assessment, these skin conditions should be considered in the plan of care, according to the RAI Manual. Coding minor skin conditions like rashes or lacerations has tripped people up before, particularly in facilities lacking a comprehensive skin care program with strong clinical support and when staff have been unable to determine accurately the skin condition or injury, says Linda M. Elizaitis, president of CMSCompliance Group Inc. in Melville, New York. “Lack of training and knowledge in wound care can impact accurate completion of this section of the MDS,” she adds. Top tips: When you evaluate surgical wounds for M1040E (Surgical wound[s]), remember these coding tips from Kim steele, Rn, WCC, RaC-Ct, CHHRP-LtC, Regional Consultant and Trainer with Harmony University and Vice President of Field Operations for Harmony Healthcare International in Topsfield, Massachusetts: o It will remain a surgical wound even if the graft and/or flap fails. How to Code The lookback for M1040 is 7 days; if none of these signs or symptoms present, simply check Z (None of the above …). In M1040, you’re simply recording, with a check, whether any of these conditions are present or have been present in the past 7 days, so you don’t have to worry about assessing the severity or documenting the number of incidences. Don’t miss these other MDS sections: Compliance tip: Surveyors are paying extra attention to pressure ulcers, but your quality measures and reimbursement can be negatively impacted by conflicting documentation, inaccurate coding, and quality of care for other skin conditions as well, says Steele. Work With Your Team Take an interdisciplinary approach for the best assessment, monitoring, and treatment, when necessary, of skin conditions. Remember that a working clinical knowledge of what to look for and how to distinguish different skin ailments is the basis for accurate MDS coding. Additionally, communication with your team members is key to coding the MDS correctly. “Nurses who do not have MDS coding responsibilities must still be aware of Section M coding instructions,” Steele says.