Don't Be Intimidated by Oral Examinations
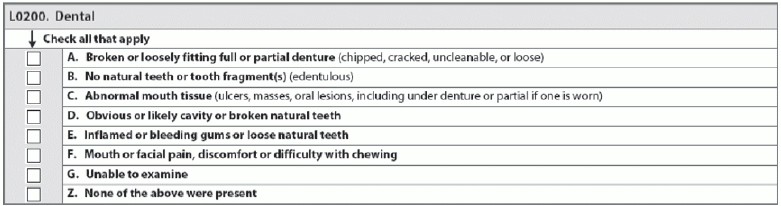
Oral health assessments and coding can bolster quality of life and Quality Measures (QM). Though dental health is often separated from bodily health in our medical culture, mouth issues can be symptomatic of issues elsewhere in the body. The oral health assessment can be crucial to evaluating a resident’s well-being. Checking in on oral health can be key to discovering underlying conditions or as an answer to mysterious changes in behavior. Even if your facility doesn’t have a dental consultant on staff and you don’t feel confident about making the assessment, evaluating a resident’s oral health is a significant aspect of ensuring resident health and care-planning. If you only have minimal dental training, section L may seem intimidating. Gaining knowledge about what a healthy mouth looks like and the best way to make a resident comfortable before attempting an assessment will help you become more confident. Coding Section L accurately establishes a baseline for each resident’s oral health. Performing the assessment makes sure that the resident receives any appropriate or necessary treatments in a timely manner. Learn Why Assessing Oral Health is Crucial A healthy mouth — teeth, gums, and tongue — is indicative of total health. Oral care can be compromised easily in SNFs because most facilities don’t have dental staff on-site, and very few medical educations offer comprehensive dental training. Beware: Quality measures like weight loss can be triggered by poor oral health. Residents with poor oral health are also at increased risk for cardiac-based diagnoses, says Renee Kinder Ms CCC-sLP RaC-Ct, Director of Clinical Education of Encore Rehabilitation in Louisville, Kentucky. Plus, residents who have some signs of poor oral health, such as bleeding gums, could indicate an issue leading to excessive extractions, which would compromise quality of life, pain, and the ability to eat. “Oral health and oral hygiene are always a huge area where we see training needs with nursing staff,” Kinder says. More training is especially important for staff who handle residents who Prepare Beforehand First, do some background research. Ask the resident whether she’s had any problems or discomfort in her mouth when at rest or when chewing. If the resident is unable to answer whether she has pain when eating, observe her during mealtimes and look for signs of mouth pain. Find out if she has dentures or partials — and if family says she does, but you can’t find any evidence at your facility, find out why. Make sure you have a light source, like a pen light, before you conduct the assessment. If the resident does have dentures, ask him to remove them before you examine her mouth. Assess the dentures for cracks, chips, and cleanliness. Are you Looking at a Healthy Mouth? The Kayser-Jones Brief Oral Health Status Examination, a product of the Gerontological Society of America, published in 1995, is an excellent graphical screening tool to examine a resident’s mouth and better understand whether what you’re seeing falls on the healthy side of the oral health spectrum. Basically, you’re looking for pink, moist surfaces (tongue, lips, gums, other tissue) that are free of food particles or excessive tartar. Both natural and artificial teeth should be smooth — not broken — and fit comfortably in the resident’s mouth, without irritating any tissue. Watch for Warning Signs Unhealthy mouths can show literal red flags. Look out for bright red hues on the tongue, lips, inside of cheeks, and gums. White splotches, too, can be indicative of disease. Any open sores or ulcers or broken teeth require a dentist’s attention immediately. Catching these problems early can save a resident a lot of pain and greatly boost their quality of life. “Ensuring problems are identified in early stages of change to prevent serious oral health and dental issues and to make referrals to dental professionals in a timely manner,” Kinder says. Code Section L Correctly To code Section L, assess and then simply make a check mark for each sub-item that applies. “What differs here from other areas of the MDS is that the assessor simply checks a box. So, there is no scale or severity attached,” Kinder says. This means that Section L as a monitoring tool is useful mostly as a baseline, and not necessarily to monitor changes.