Stumped On A1500- A1550? Here's Your PASRR Primer
Don’t throw away Level II screen at the first hint of dementia diagnosis.
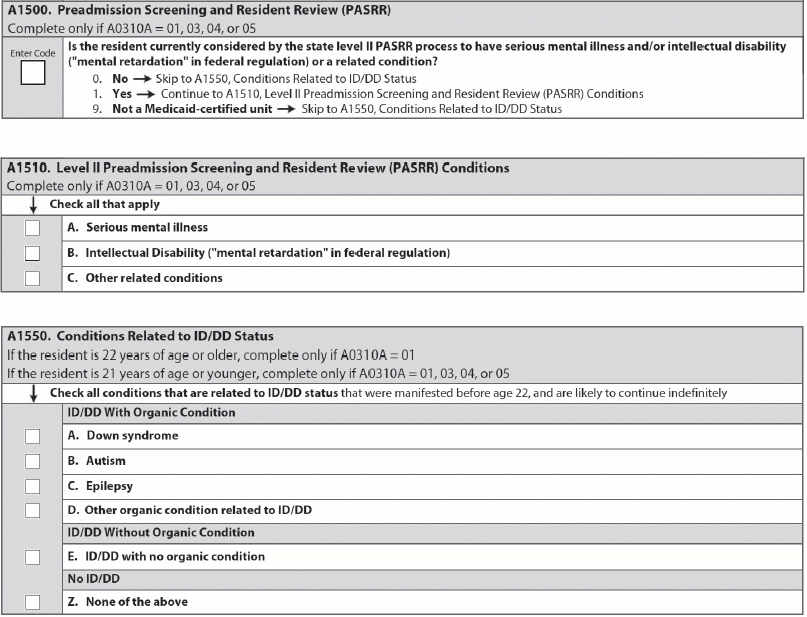
There are a lot of moving parts when it comes to coding item A1500 — Preadmission Screening and Resident Review (PASRR). And depending on your state’s regulations and your facility’s staffing, you may be working with multiple people to correctly code this section of the MDS. Here is some sage advice to shine a light on PASRR and the MDS.
What PASRR Means for MDS Coding
Background: PASRR is a preadmission screening process for individuals with mental illness or mental retardation. Each resident admitted to a Medicaid certified bed, or a dually certified bed (Medicare and Medicaid), must have a PASRR, according to the Missouri Department of Health & Senior Services (MDHSS).
Impact: Approximately 10 percent to 25 percent of nursing facility residents have serious mental illness, mental retardation or a related condition, notes the North Carolina Department of Health and Human Services (NCDHHS). “Historically, these individuals have been inappropriately placed and underserved. PASRR is a powerful tool for diversion or transition to the most appropriate available service setting.”
Typically, a resident will need a PASRR for his first admission to a nursing facility or after the resident has been out of a nursing facility for 60 days or longer, MDHSS says.
“A positive screen indicates that the resident has a mental illness, mental retardation, or a related condition,” explains NCDHHS. And for A1500, you’re documenting whether a PASRR Level II determination has been issued.
According to MDHSS, triggers for Level II screening include:
How Change in Status Affects PASRR
Tip: “Whenever a Significant Change in Status Assessment is triggered, look at A1500,” NCDHHS advises. If A1500 is YES, follow your state’s PASRR procedures for referral for Level II screening.
A Change in Status PASRR application is allowed only when the resident is previously approved for nursing facility placement and has been out of a nursing facility for more than 60 days, MDHSS explains. Keep in mind that a Significant Change in Status is a change in two or more areas on the MDS 3.0 regarding a resident’s needs, and these changes can be either physical or mental.
Example: The resident has had inpatient psychiatric treatment in the last two years, which is a trigger for the Level II screening. The resident has had the initial preadmission screening and was admitted to the nursing facility. The resident then goes to the hospital for medical, physical and/or psychiatric reasons, and then is readmitted to the original nursing facility. In this case, you must assess the resident for a Change in Status and submit the PASRR application if necessary.
And as with any condition, if the need is urgent, don’t hesitate to immediately refer the resident for PASRR and/or services, NCDHHS urges. For example, you may have a resident who is experiencing an acute change in affect or behavior that doesn’t call for hospitalization but needs evaluation and a change in the care plan.
Beyond A1500: Quick Tips
Next step: For item A1510, you need to document the Level II PASRR conditions, meaning what findings the screening yielded in the resident. You have three choices:
A. Serious mental illness
In A1550 — Conditions Related to ID/DD Status, you must document the conditions associated with the resident’s MR or DDs, NCDHHS instructs. Be sure to check all conditions related to MR/DD status present before age 22. And when the age of onset isn’t specified, “assume that the condition meets this criteria AND is likely to continue indefinitely.”
Caveat: When Dementia is the Primary Diagnosis
One snag with PASRR that has caused some confusion is the PASRR regulations’ loophole that allows termination of Level II screening if the individual has a primary diagnosis of dementia or a non-primary diagnosis of dementia without a primary diagnosis that is a serious mental illness, MR/DD, or related condition.
“Partly because of its awkward phrasing, this part of the CFR has generated a great deal of confusion among state staff who work on PASRR,” according to the PASRR Technical Assistance Center. “Anecdotally, it would appear that evaluators in many states terminate PASRR as soon as they detect any evidence of dementia.” But this would be wrong.
In fact, the intent of this provision in the regulation is to end the Level II screening when the individual would not benefit from mental illness or MR/DD services provided under a nursing facility’s per diem or from specialized services provided in the facility or other institutional setting, the Center explains.
What to do: When there is a primary diagnosis of dementia, even if the individual meets all the other criteria, do not refer for Level II, instructs the Kansas Department for Aging and Disability Services (KDADS). But when an individual has a diagnosis of dementia that is not primary and meets all the other criteria to need a Level II screening, you should refer the resident for this screening.
Don’t Get Duped by Hospital Staff
Another problem is when hospital discharge planning staff tell you that “no Level II is needed.” Don’t fall into this trap.
“We have had indications that some [hospital staff] communicated this to nursing homes considering admission of a resident,” KDADS says.
“Physicians sometimes indicate that dementia is primary because they wish to accelerate the process of nursing home admission (especially for families experiencing acute distress), and they know that a diagnosis of primary dementia will ‘short-circuit’ PASRR,” the Center points out.
Bottom line: “Remember, it is the nursing home that is held accountable to complete PASRR appropriately, not the hospital,” KDADS stresses. So don’t arbitrarily go along with hospital staff’s recommendations to skip the Level II screening.
B. Intellectual Disability (“mental retardation” in federal regulation)
C. Other related conditions