MDS Changes Coming October 2018
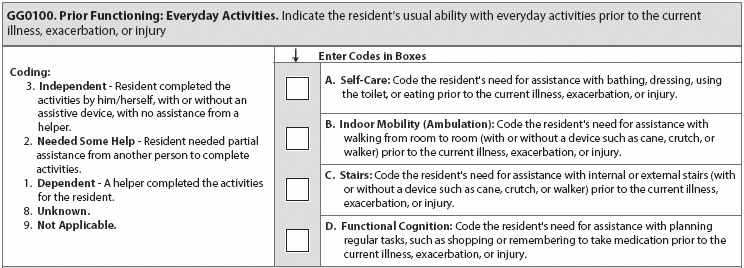
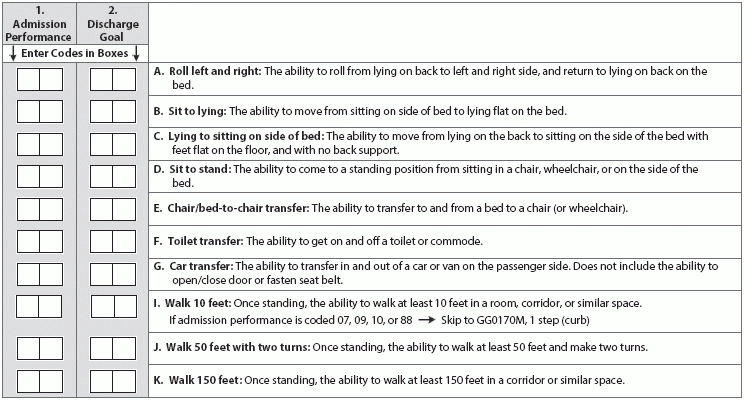
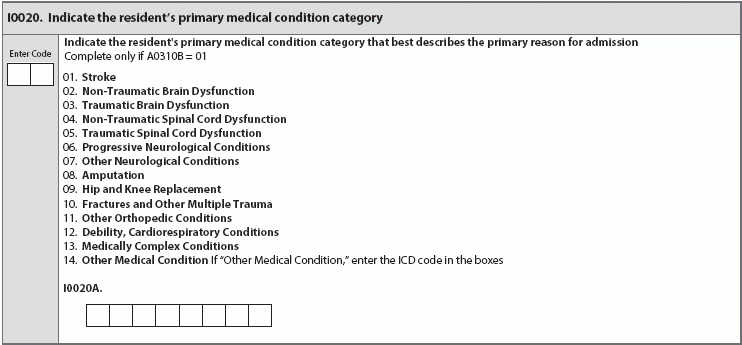
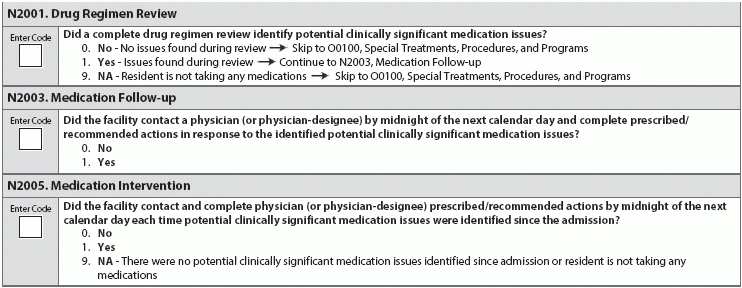
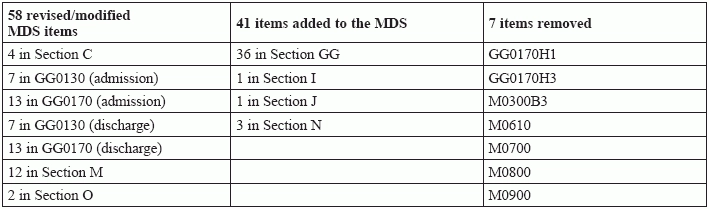
The 106 changes include new item sets requiring IDT collaboration. Though the 2019 MDS is still in draft form, start preparing now for the 106 changes in MDS item sets, including 58 revised or modified MDS items, 41 additions, and seven removals. Jessie McGill Rn, RaC-Mt, curriculum development specialist at the American association of nurse assessment Coordination (AANAC) in Denver, recently led a webinar highlighting the clarifications, additions, and removals affecting the next iteration of the MDS. Here are some of the biggest changes to keep in mind. Section A(Identification Information) One big change: The Centers for Medicare and Medicaid Services (CMS) is taking the requirement for a social security number off of all MDS forms, beginning April 2018, in lieu of a Medicare Beneficiary Indicator (MBI). From April 2018 to Dec. 31, 2019, facilities should use the health insurance claim number or MBI. By Jan. 1, 2020, all claims submitted to Medicare must have the patient's MBI. This change affects item A0600 (Social Security Number and Medicare Numbers). Hint: The removal of the social security number should make the MDS less sensitive and easier to manage, cybersecurity-wise. Section GG (Functional Abilities and Goals) There are three big additions to Section GG, including the addition of items assessing prior functioning, self-care, and mobility. These additions can be traced back to skilled nursing facility (SNF) quality reporting program (QRP) requirements. The QRP quality measurements have four new section GG outcome measures. Assessments will now include more specific quantifiable ambulation, as required in new subitems in GG0170 (Mobility). The changes suggest that CMS is recognizing that residents aren't necessarily facility-bound, and hint that documentation of maintenance of function will be prioritized as much as loss of function. Evaluate Prior Functioning While the RAI Manual updates will have further guidance and instruction on how to evaluate a resident's prior functioning, it's probably safe to assume that you can rely on interviews with the resident, her family or representative, and any clues you can ascertain from the recent clinical record. "We really need to see what the RAI manual will instruct us .... Ultimately, the hospital staff may be able to assist, or we may need to use dashes for information not available. We need to do the best we can to find out prior function, but if we can't get the information, then we will have to dash the lines," an AANAC representative said, during the webinar. The complexity of new items in Section GG all have therapy highly involved, McGill says. Start preparing to document these new MDS requirements by making sure your therapy department will be closely involved in how you will assess these items, so you'll be ready come October, she adds. Changes to Mobility New subitems in GG0170 (Mobility) better measure ambulation and independence, including changes in how to assess mobility, by measuring the resident's ability to move instead of the distance the resident is able to cover: 1 step (curb), 4 steps, and 12 steps. Another noteworthy change is the addition of a subitem assessing whether a resident can stoop or bend over to pick up an object. Your facility and team may find that your therapist team members' input is more crucial than ever when assessing and documenting these changes. "A therapist can complete the MDS sections that they are assigned to respond to. The facility can determine who will complete which sections of the MDS. If the nurse is going to use the information that the therapist provides, that is an acceptable approach as well. Again, you will need to determine who is responsible to complete each section of the MDS. Regarding section GG, you may want to collaborate as a team to complete the section to be sure to include all IDT perspectives," an AANAC representative said, during the webinar question and answer session. Also look out for the addition of subitem GG0170G (Mobility, Car transfer) which aims to evaluate whether a resident can "transfer in and out of a car or van on the passenger side. Does not include the ability to open/close door or fasten seat belt" upon both admission and discharge. Section I(Active Diagnoses) Look out for a new item on the comprehensive, PPS, quarterly, and swing-bed PPS) MDS assessment types: Item I0020 (... Resident's primary medical condition category), which provides a space for the NAC or assigned team member to note whether a resident has a medically complex condition or other orthopedic condition or debility, choosing from the conditions provided by the list or listing the appropriate ICD-10 code in I0020A. Note that these new items will only be coded on the aforementioned assessment types if A0310B (PPS Assessment for a Part A Stay) is coded 1 (5-day scheduled assessment PPS). The RAI Manual updates will hopefully provide more guidance on how to describe primary reasons for admission stay. A good note to remember, when preparing to code I0020, is that a condition is not how you or staff or CMS defines it, but how the RAI User's Manual defines it, McGill says. Note: Section I (Active Diagnoses) will correspond with the potential change in payment methodology for Medicare residents, too, says Marilyn Mines, Rn, BC, RaC-Ct senior manager at Marcum LLP in Deerfield, Illinois. For more on the Resident Classification System, Version 1 (RCS-1), see page 30. Section J (Health Conditions) New addition of item J2000 (Prior surgery) for the 5-day PPS assessment, to scope out whether residents have had major surgery in the 100 days prior to admission. Section M (Skin Conditions) Though reasons have not yet been provided, CMS will delete the following Section M (Skin Conditions) items, leaving a very different Section M: Keep an eye out for the RAI Manual updates to see how these deletions will affect Care Area Triggers (CAT). McGill says CMS will not be adding new triggering conditions, and the pressure ulcer CAT will continue to use the remaining nine triggering conditions. There will be other clarifications in language in Section M (Skin Conditions), as well, to make sure items and their descriptions and instructions use current National Pressure Ulcer Advisory Panel (NPUAP) terminology. Note: The removal of these items and adjustment of CAT will affect quality measures for the short stay MDS 3.0. The QM numerator uses M0800A, B, and C. Section N(Medications)There are three item changes in Section N (Medications): the addition of N2001 (Drug Regimen Review), N2003 (Medication Follow-up), and N2005 (Medication Intervention). These items may catch potentially significant medication issues as a resident is admitted into a skilled nursing facility from a post-acute care setting. "According to the MDS item set, we have until midnight on the next calendar day after an issue was identified to clarify the medication issues and deal with any discrepancies in N2003," an AANAC representative said during the webinar. "If the resident admits and we are clarifying the medication orders, then to comply, we would need to respond to discrepancies quickly. We hope to have more instructions in the revised RAI manual later this year." Resource: Until the RAI Manual updates are released, you can find more information on how drug regimen review should be conducted and assessed in the State operations Manual appendix PP, released November 2017, under F756 §483.45(c) Drug Regimen Review. Though the drug regimen review itself must be conducted by a licensed pharmacist, per Appendix PP guidance, the MDS item N2001 (Drug Regimen Review) "can be completed by professionals determined by the facility to be competent to complete the sections," said an AANAC representative during the webinar. "An MDS nurse may complete it with input from the nurse manager and pharmacists, but it's up to the facility to determine who is skilled and competent to complete the section," the representative said. Recap: This is a breakdown of the changes you can expect to see in the next version of the MDS, effective Oct. 1, 2018.