Reduce Logic-Check Warning Messages With Proper Admission Coding
Why Item A1900 is giving many providers headaches.
If you’re getting logic check error messages while coding Section A — Identification Information of the MDS, you may be coding the admission items wrong. And with all the recent changes to admission coding, it’s pretty easy to make mistakes. Here’s where you’re likely running into problems — and how to enter the admission data without getting warning messages.
Watch Out for Software Roadblocks
Problem: If the start date of the current SNF stay and the current episode of a stay do not agree in a logic check performed by the software, you will get an error message and won’t be able to close the assessment until you resolve the logic conflict, according to a May 21 blog posting by Beckie Dow, vice president of field operations for Topsfield, Mass.-based Harmony Healthcare International.
This “warning message” is in place to assist providers in correcting logic conflicts before submitting assessments to the Quality Improvement and Evaluation System (QIES) Assessment Submission and Processing (ASAP), Dow explained. This decreases the number of rejected assessments during submission.
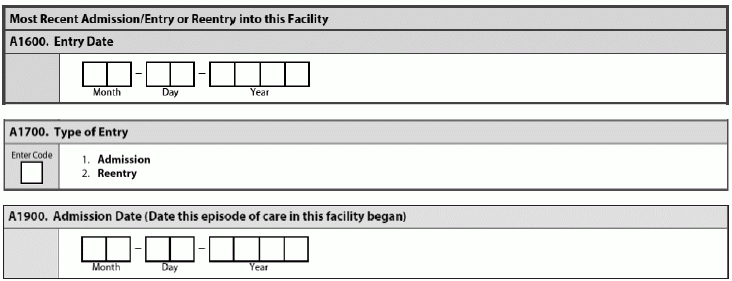
The October 2014 release of the updated RAI Manual, and then the subsequent February 2015 revision, made significant changes to Section A of the MDS 3.0 — and some of these changes are in conflict during the logic check, Dow noted. With these changes, and the addition of Item A1900 — Admission Date (Date this episode of care in this facility began), now coding in Items A1600, A1700 and A1900 “are closely linked.”
That’s why “software logic checks between these items may result in a warning message that will prompt the provider to correct the logic error before the assessment will ‘lock’ and be available for submission,” Dow explained.
Know Your A1600 — A1900 Coding Rules
The entry date that you code in Item A1600 — Most Recent Admission/Entry or Reentry into this Facility is the initial date of admission to your facility, or the most recent date of admission/entry or reentry into your facility, according to a recent presentation by Shirley Boltz, RN, RAI/Education Coordinator for the Kansas Department for Aging and Disability Services (KDADS).
Do this: To properly code Item A1700 — Type of Entry, you should identify whether the entry date in A1600 is an Admission date or a Reentry date, Boltz said. You should code 1 — Admission in A1700 if one of the following occurs:
Or, code 2 — Reentry for Item A1700 if all three of the following occur prior to this entry:
Remember: And keep in mind that you do not count the discharge date in the 30 days, Boltz stressed. Both swing bed facilities and nursing homes must follow these rules.
Why Item A1900 is Easy to Blunder
Item A1900 “causes providers confusion because of the concepts of ‘stay’ and ‘episode,’ which are made clear in the Quality Measures User’s Guide but are not always correctly referenced to the RAI User’s Manual,” Dow cautioned. But always stick to the rule of thumb that the date you code in Item A1900 should remain the same for all assessments in a given episode, even if the episode is interrupted by temporary discharges from your facility.
However, if the resident returns after a discharge return not anticipated, or if more than 30 days pass after the resident’s discharge, a new episode will begin and you will code A1900 with the new admission date, Dow noted.
Pay attention: The February 2015 version of the RAI Manual does, however, offer many Coding Tips and clarifies the concept of a “stay” versus an “episode.” Page A-26 of the RAI manual states:
“A stay is a set of contiguous days in the facility and an episode is a series of one or more stays that may be separated by brief interruptions in the resident’s time in the facility. An episode continues across stays until one of three events occurs: the resident is discharged with return not anticipated, the resident is discharged with return anticipated but is out of the facility for more than 30 days, or the resident dies in the facility.”
Learn from This Coding Example
Scenario: This is Mr. Smith’s first admission to your facility. Upon his admission, you will complete an entry tracking record, and the dates that you enter into Items A1600 and A1900 will match. You will code A1700 as 1 — Admission. “This coding will remain constant for all subsequent assessments within the first stay in that episode,” Dow instructed.
“If the resident is discharged return anticipated and reenters the facility within 30 days, a new stay will begin,” Dow said. “However, the current episode will continue.”
Upon readmission, you would complete another entry tracking record and you would change the date in A1600 to the new reentry date. Code Item A1700 as 2 — Reentry. Then, make sure Item A1900 continues to show the original admission date, which is also the date that the first day of this care episode began, Dow explained.