Refresh Your E0100 & E0200 Coding To Properly Record Resident Behaviors
Make sure you’re taking these extra steps to assess possible delusions in E0100.
While you’re getting comfortable with coding the new item C1310 — Signs and Symptoms of Delirium (from CAM ©), there is no better time to brush up on your coding of some tricky items in Section E — Behavior. Plus, your coding of item E0200 — Behavioral Symptom — Presence & Frequency will have a huge impact on your quality scores for one of your long-stay measures.
Understand Hallucination & Delusion Definitions
Definitions: The RAI Manual breaks down the psychosis indicators for item E0100 — Potential Indicators of Psychosis into two categories:
Psychotic symptoms may be associated with delirium and dementia, but they may also be linked to adverse drug effects, psychiatric disorders, or hearing or vision impairment. To assess for item E0100, the RAI Manual instructs you to review the resident’s medical record for the seven-day look-back period, as well as interview staff and others about the resident’s behavior.
You should also observe the resident during conversations and assessment interviews to listen for statements indicating experiences of hallucinations or delusions.
Important: The RAI Manual sets out an additional step for assessment, in which you need to clarify potentially false beliefs (delusions):
Mistake: If you cannot objectively show a belief to be false, or if it’s not possible to determine whether a belief is false, do not code this as a delusion. Additionally, if a resident expresses a false belief but easily accepts a reasonable alternative explanation, do not code it as a delusion.
Learn from 3 Psychosis-Indicator Scenarios
Here are a few E0100 coding examples from the RAI Manual that are helpful in demonstrating proper coding:
Scenario 1: Staff have found Mrs. Jones speaking aloud in her room, but no one is present and staff note that they heard no other voices in the environment. When » » » asked about this, Mrs. Jones states that she is answering a question posed to her by the gentleman in front of her.
How to code: For this scenario, you would check E0100A — Hallucinations. Because the resident reports auditory and visual sensations that occur in the absence of any external stimulus, this is a hallucination.
Scenario 2: Mr. Smith announces that he must leave to go to work, because he’s needed in his office right away. When staff reminded Mr. Smith that he’s been retired for 15 years, he continues to insist that he must get to his office.
How to code: Check E0100B — Delusions. In this case, Mr. Smith sticks to the belief that he still works, even after you’ve reminded him about his retirement status. Because he holds the belief firmly despite an explanation of the real situation, this is a delusion.
Scenario 3: Mrs. Brown believes she must leave your facility immediately because her mother is waiting for her to return home. Staff know that Mrs. Brown’s mother is deceased and gently remind her of this. In response, Mrs. Brown acknowledges, “Oh yes, I remember now. Mother passed away years ago.”
How to code: For this scenario, you would check E0100Z — None of the above. Mrs. Brown readily corrects her initial false belief after a simple reminder, which suggests that her mistaken belief is due to forgetfulness or memory loss rather than psychosis. Because this is not a firmly held false belief, it does not fit the definition of a delusion.
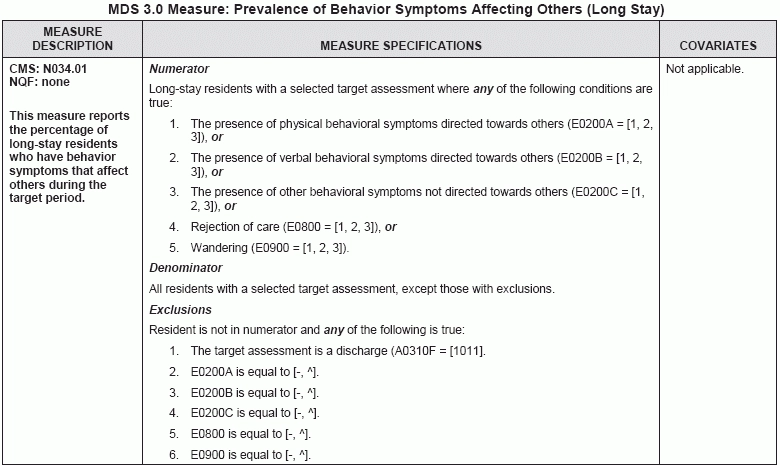
Improper E0200 Coding Will Impact Quality Scores
Another important item in Section E is E0200 — Behavioral Symptom — Presence & Frequency. Your coding of item E0200 plays a key role in scoring the quality measure “Prevalence of Behavior Symptoms Affecting Others (Long Stay).”
To assess item E0200, you must review the medical record for the seven-day look-back period and observe the resident in a variety of situations during the period. You must also interview staff across all shifts and disciplines, as well as other who had close interaction with the resident during the look-back period, such as family or friends.
Item E0200 has three sub-items:
1. E0200A — Physical behavioral symptoms directed toward others (e.g., hitting, kicking, pushing, scratching, grabbing, abusing others sexually);
Caveat: Note that E0200C does not include wandering — instead, you should code this behavior in item E0900 — Wandering — Presence & Frequency.
Best bet: You should code E0200 based on whether the symptoms occurred, and not based on how you would interpret the behavior’s meaning or cause. Even if staff have grown accustomed to the behavior or view it as typical or tolerable, you should still code it as present.
Let These E0200 Examples Show You the Way
Still a little foggy on how to properly code E0200? The RAI Manual provides the following examples to illustrate correct coding of item E0200:
Scenario 1: Staff have previously found Mrs. Reynolds rummaging through the clothes in her roommate’s dresser drawers. But staff have not observed this behavior, nor have others reported this behavior, in the last seven days.
How to code: For this scenario, you would code E0200C as 0 — Behavior not exhibited, because the behavior did not occur during the look-back period.
Scenario 2: Mr. Shaw throws his dinner tray at another resident who repeatedly spit food at him during dinner. This is a single, isolated incident.
How to code: Code this scenario in E0200A as 1 — Behavior of this type occurred 1 to 3 days. Although there is a possible explanation for Mr. Shaw’s behavior, throwing a tray was still a physical behavior directed toward others and you must note the behavior as present because it occurred.
Scenario 3: Every morning, a nursing assistant tries to help Mr. Green who is unable to dress himself. On the last four out of six mornings, Mr. Green has hit or scratched the nursing assistant during attempts to help dress him.
How to code: You would code E0200A as 2 — Behavior of this type occurred 4 to 6 days, but less than daily, because scratching the nursing assistant was a physical behavior directed toward others.
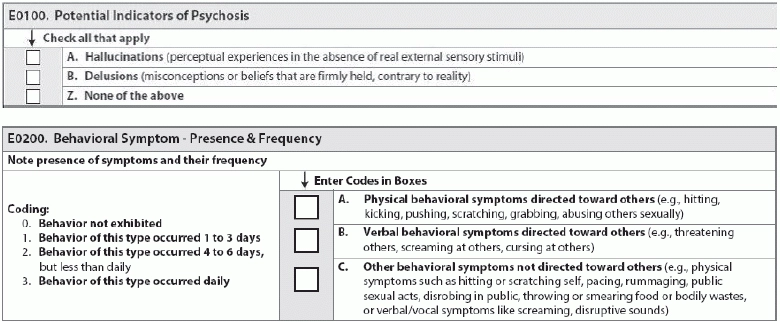
2. E0200B — Verbal behavioral symptoms directed toward others (e.g., threatening others, screaming at others, cursing at others); and
3. E0200C — Other behavioral symptoms not directed toward others (e.g., physical symptoms such as hitting or scratching self, pacing, rummaging, public sexual acts, disrobing in public, throwing or smearing food or bodily wastes, or verbal/vocal symptoms like screaming, disruptive sounds).