Highlight These Fibroid Removal, Myomectomy, Colporrhaphy Edits To Avoid Denials

You can potentially appeal denials you received for this revision.
April brings more than May flowers, as you’ll have to contend with the National Correct Coding Initiative (CCI) version 22.1’s new edits, all of which went into effect April 1, 2016. They include edits affecting fibroid removal, myomectomy, and combined anteroposterior colporrhaphy procedures.
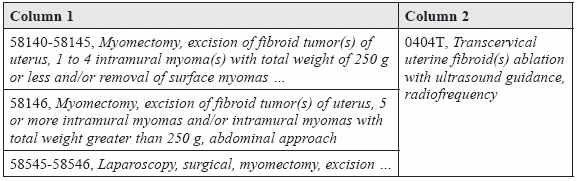
Limit Your Fibroid Removals to One Type
The edits listed below basically state that only one type of fibroid removal procedure should be billed for the same surgical session, explains Melanie Witt, RN, MA, an independent coding expert based out of Guadalupita, N.M.
Can you use a modifier? The edits have a modifier indicator of “1,” which means that you can use a modifier to bypass this bundle, but the documentation would have to clearly show that there was a combination of excision and secondary use of radiofrequency, which is highly unlikely. Also, note that the bundled code is a Category III CPT® code which may cause a denial if the payer policy is to only pay for Category 1 CPT® codes.
Additionally, the following four codes have been bundled into all of the gyn and ob procedure codes. These edits carry a modifier indicator of “1,” saying that this is a “misuse of column two code with column one code.” This is because IV infusions are usually part of a surgical procedure. Here are the bundled codes:
Deleted/Revised Edits effective April 1, 2016
Deletion: You should delete the previous edit that bundled 57260 (Combined anteroposterior colporrhaphy) into:
These edits carried a “0” indicator, which meant that 57260 could not be billed together with any of these codes under any circumstances. This bundle was first initiated on January 1, 2014, and the effective date of the deletion is April 1, 2016, but it may be possible for practices to appeal if this code combination was denied between these dates — even though it is clear that Medicare carriers will not be adjusting any of these denials automatically.
Revision: In addition, effective April 1, 2016, CMS changed the bundling indicator for codes 57280 (Colpopexy, abdominal approach) and 57283 (Colpopexy, vaginal; intra-peritoneal approach [uterosacral, levator myorrhaphy]) from a “0” to a “1” when billed with the following CPT® codes:
Remember that use of a modifier 59 (Distinct procedural service) or one of the new “X” modifiers must be supported by the documentation.