You Need to Have a Sense of What’s Routine—And What Isn’t—For Multiple Gestations
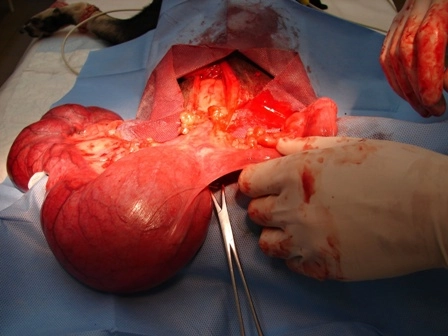
If your ob-gyn delivers multiple babies via c-section, apply this modifier. When a patient presents to your office with a multiple gestation pregnancy (twins, triplets, etc.), it’s up to you to know how to report this specific kind of obstetrical care — including additional complications. Will you be ready? First step: As with any pregnancy with complications, your first step should be to determine what E/M care the ob global package includes and what may be considered above and beyond -- and therefore separately billable from the global. Bottom line: Each insurance carrier generally outlines a specific number of visits that it considers part of the global package, which is usually 12 or 13. If the patient has more than the prescribed number of visits and you have documentation backing up the medical necessity for the extra visits, you should charge these outside the global ob fee. Be sure to link any care for the mother and/or fetuses to the appropriate ICD-10-CM codes. For the delivery, the code categories for the mother’s record are O30.- (Multiple gestation…) and Z37.- (Outcome of delivery…), and for the babies’ record are P01.5 (…Multiple pregnancy) and Z38.3- through Z38.6- or Z38.7- or Z38.8- (Other multiple liveborn infant …). More Fetuses Mean More Complications Several complications are inherent in multiple gestation pregnancies, says Sarah Holmes, MAL, CPCO, CMM, HITCM-PP, executive administrator and medical coding and billing instructor at Clayton State University in Decatur, Georgia. For example, ob-gyns automatically consider any such pregnancy as high risk. They involve a number of additional prenatal visits and significantly more monitoring because the physician has to pay attention not only to the mother’s health but also to the growth rate and condition of all the fetuses. Specifically with multiparities, the ob-gyn must closely monitor the mother’s blood pressure levels, as well as fetal growth. Typically, this extra care can involve such procedures as fetal non-stress tests (NSTs, 59025, Fetal non-stress test), biophysical profiles (76818, Fetal biophysical profile; with non-stress testing; or 76819, ... without non-stress testing) and several ultrasounds to monitor the growth of each baby. For example, a patient pregnant with triplets has 15 prenatal visits (not that far outside the normal routine global period), but she receives four ultrasounds and several injections of Celestone Soluspan to prevent respiratory problems in the fetuses. You should report these items separately from the global period. Report the first ultrasound as 76801 (Ultrasound, pregnant uterus, real time with image documentation, fetal and maternal evaluation, first trimester [< 14 weeks 0 days], transabdominal approach; single or first gestation) and two listings of +76802 (... each additional gestation [List separately in addition to code for primary procedure]), or 76805 (Ultrasound, pregnant uterus, real time with image documentation, fetal and maternal evaluation, after first trimester [> or 14 weeks 0 days], transabdominal approach; single or first gestation) and two units of +76810 (... each additional gestation [List separately in addition to code for primary procedure]), depending on the fetuses’ age at the time of the ultrasound. For each subsequent ultrasound, you should use 76816 (Ultrasound, pregnant uterus, real time with image documentation, follow-up [eg, re-evaluation of fetal size by measuring standard growth parameters and amniotic fluid volume, re-evaluation of organ system[s] suspected or confirmed to be abnormal on a previous scan], transabdominal approach, per fetus). Report 76816-59 (Distinct procedural service) for each additional fetus examined in a multiple pregnancy that is evaluated, CPT® states. In addition, you would report the Celestone Soluspan injections with along with J0702 (Injection, betamethasone acetate 3 mg and betamethasone sodium phosphate 3 mg). Don’t Forget Extra Work at Delivery Despite the focus on prenatal care, things can get more complicated when the time comes to deliver all those babies. Such births involve more operating room time to coordinate, extra personnel to receive the babies as they deliver, increased chances for bleeding problems, and frequently a cesarean birth. If the patient is having twins, most physicians try for a vaginal delivery if everything looks in order. Here you should report 59400 (Routine obstetric care including antepartum care, vaginal delivery [with or without episiotomy, and/or forceps] and postpartum care) for the first baby and 59409-51 (Vaginal delivery only [with or without episiotomy and/or forceps]; multiple procedures) for the second. If the ob-gyn delivers the first baby vaginally but the second by cesarean, you should report 59510 (Routine obstetric care including antepartum care, cesarean delivery, and postpartum care) for the second baby and 59409-51 for the first. When the doctor delivers all of the babies (that is, twins, triplets, quads, etc.) by c-section, you should report 59510 with modifier 22 (Increased procedural services) appended. In this case, include a letter with the claim that outlines the additional work involved in the multiple deliveries to give the carrier a clear picture of why you’re asking for additional reimbursement. Special Rules Apply if Specialist Gets Involved Occasionally, a multiparity patient’s ob-gyn will send her to a maternal fetal medicine (MFM) specialist for consultation and possible monitoring of the pregnancy. If the MFM specialist takes over the monitoring (i.e., care of the patient is transferred to the MFM for the rest of the pregnancy), that means two physicians are billing for ob care. Neither doctor will be able to report global care, unless the insurance carrier insists. If the patient is seen only for intermittent care with an MFM, the attending OB may be allowed to bill globally, with the MFM billing each visit separately. But only one ob will charge for the delivery. If both physicians are present at the delivery and global billing is not permitted, one will bill as the primary surgeon (59409 or 59410 for vaginal delivery and 59514 or 59515 for c-section), and the other will report as an assistant surgeon (59409-80 [Assistant surgeon] for vaginal and 59514-80 for cesarean), says Ashley Zyduck, CPC, CPB, CENTC, COBGC, lead physician coder for Medkoder in Jackson, Missouri. With both an ob and a specialist seeing the patient, payers may accept only itemized billing. Or they may allow the primary doctor to report the global ob code with or without a modifier 52 (Reduced services) appended. Correct coding also may depend on who will be providing the postpartum care because you may have to choose between 59409 and 59410 (... including postpartum care) or 59514 and 59515 (... including postpartum care). In any case, you should check with the patient’s insurance provider to determine how it would best like the ob services to be reported.