Brenda1973
Networker
- Messages
- 94
- Best answers
- 0
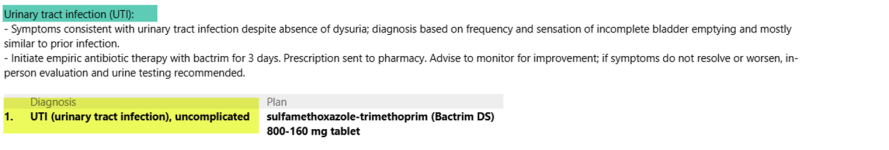
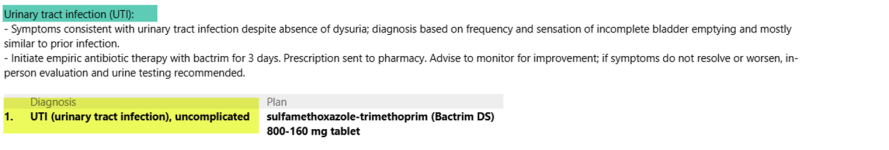
Hello! please help. My provider is stating that his definitive diagnosis is UTI . I feel that he needs to remove the "symptoms consistent with" as that phrase is no longer allowed according to outpatient coding guidelines updated in 2020. The green highlight use to be the "Assessment" in the SOAP note but he has deleted the word assessment and added his diagnosis there and again in yellow as his final diagnosis. Please advise me as the guidelines state "consistent with" is not valid for a final definitive diagnosis. Can it be documented in the body of the note? can it be documented in the assessment and still use as a final diagnosis? My understanding has always been that the assessment is where we find the final diagnosis, so with that documentation in the assessment I would not be able to use UTI. I need a documentation expert here! Thanks!