To be clear you are referring to BCBS of Alabama, correct? I'm making that assumption based on your location being listed as Alabama. If it isn't BCBS of Al, which BCBS is it giving you problems?
Also, since the services for providing a depo injection are separately billable from an office visit/E&M, they aren't obligated to cover the visits per the following snip in BCBS of AL's
Preventive Care Services under Healthcare Reform policy # MP-447. This policy was last reviewed in January 2023.

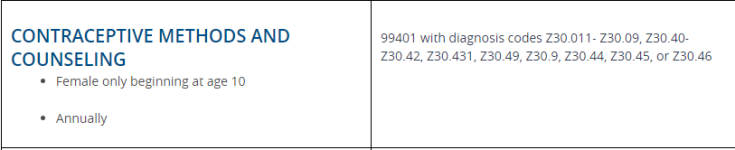
Bear in mind, included in the insurance companies' ability to apply cost-sharing to the office visit, they can also impose other limitations, such as visit maximums or frequencies (see the section highlighted in purple), because the mandate to cover the preventive service is applicable to the procedure codes which represent the mandated covered preventive services.
In the header of this document there is a link to BCBS of AL's preventive care services coding guidelines document title
Healthcare Reform, see link. In the 2nd table titled "Women's Preventive Screenings" There are a copy of lines that your office visits were being reimbursed under before these sudden denials. I included the line related to Well Woman Preventive Office Visits because you mentioned in your original post that one of the 4 annual injections are given during their annual visit, there are 3 separate lines under this benefit with the benefit listed based on the coding and each has its own frequency limitation.

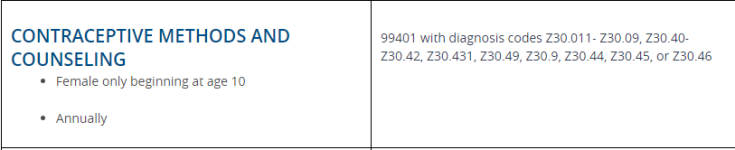

I don't see anywhere in these coding guidelines coverage listed for an E&M 99213/99214 w/DX Z30.9, and it looks like this document was updated in 10/23 based on the teeny tiny annotation "LR 10/23"in the lower right-hand corner of the document. This probably stands for "last reviewed 10/23". I say this as someone who works for a "Blue" plan myself and my familiarity with some of the strange codes included in documents that seem to mean nothing to the users.
After all of this information being tossed at you in my post, I'm going recommend you contact BCBS of AL to find out why they are suddenly denying these visits, did they have a change in policy? Did they have a system upgrade and maybe there was an issue with the upgrade that is mistakenly causing these services to deny. You'll only know whether you can get reimbursed by BCBS of AL for these services by calling them and seeing why they are denying and is there anything you can do to get them reimbursed.
Good luck!