medicalauditor
Networker
I am auditing a dermatologist, and I have this scenario: The dermatologist (Dr. A) is billing CPT code 77401 for performing SRT, and Dr. A also bills CPT code 77336 for medical physics consultation. Both chart notes are signed off by Dr. A. I am assuming that the SRT was actually done by a radiation therapist but is billed under Dr. A as incident-to, however there is no documentation of who the radiation therapist is, or of the service being incident-to - the chart looks like Dr. A did the SRT and is signed off by Dr. A. Also, the chart note for the medical physics consultation states that the consultation is being provided "per the request of Dr. A" implying that someone other than Dr. A is actually doing the medical physics consult, but the note is signed off by Dr. A and also billed by Dr. A. There is no mention of the physicist who did the consult. I am not too familiar with oncology so would appreciate some help here. My first question is:
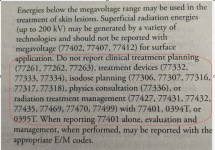
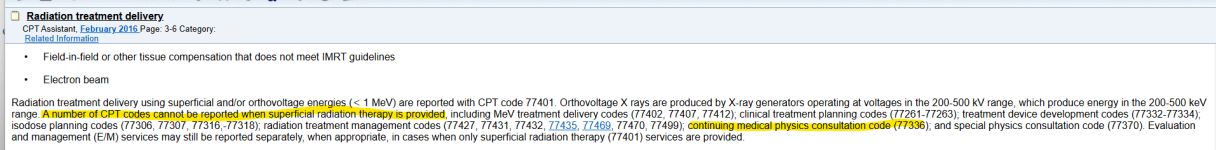
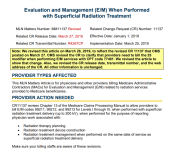
1. Considering that the 77336 code description states that the service is "in support of the radiation oncologist", can this be billed by the same provider who is doing the SRT? Even if the people doing the SRT and the med physics are 2 different people, can the 2 services be billed by the same provider?
2. Secondly, how should the 2 services be documented and who should be signing off on them?
3. Does 77336 even apply to SRTs?
4. Can you please provide a link to the CMS/Medicare resource which provides the guidelines and documentation requirements?
Thank you so much.
1. Considering that the 77336 code description states that the service is "in support of the radiation oncologist", can this be billed by the same provider who is doing the SRT? Even if the people doing the SRT and the med physics are 2 different people, can the 2 services be billed by the same provider?
2. Secondly, how should the 2 services be documented and who should be signing off on them?
3. Does 77336 even apply to SRTs?
4. Can you please provide a link to the CMS/Medicare resource which provides the guidelines and documentation requirements?
Thank you so much.