rsager1985
Contributor
I work for an FQHC and we've never been able to get Medicare to send two payments for the same date of service for the same patient. We're not trying to double dip, it's just that some of our patients will sometimes see two different providers at our clinic on the same day (vision/medical, or mental health/medical).
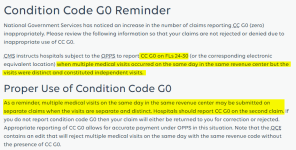
According to MLN Matters Article SE1039, "Effective January 1, 2011, two services lines are submitted with a 052X revenue code and one line contains modifier 59. Modifier 59 signifies that the conditions being treated are totally unrelated and services are provided at separate times of the day, e.g., treatment for an ear infection in the morning and treatment for injury to a limb in the afternoon." I interpreted this as meaning that we have to put a modifier 59 on one of the E/M codes to get Medicare to pay additional money for the second visit. I've tried this on dozens of claims, and they've all rejected as duplicate claims. I've called our contractor (Novitas Solutions) and they had the claims reprocessed many times, only for them to reject again and again for the same reason.
According to MLN Matters Article MM8863, the XE modifier can be used to indicate "A Service That Is Distinct Because It Occurred During A Separate Encounter." I've tried using the XE modifier to no avail.
Has anyone else had this same issue? Is it possible to get two payments when multiple encounters occur on the same date of service?
According to MLN Matters Article SE1039, "Effective January 1, 2011, two services lines are submitted with a 052X revenue code and one line contains modifier 59. Modifier 59 signifies that the conditions being treated are totally unrelated and services are provided at separate times of the day, e.g., treatment for an ear infection in the morning and treatment for injury to a limb in the afternoon." I interpreted this as meaning that we have to put a modifier 59 on one of the E/M codes to get Medicare to pay additional money for the second visit. I've tried this on dozens of claims, and they've all rejected as duplicate claims. I've called our contractor (Novitas Solutions) and they had the claims reprocessed many times, only for them to reject again and again for the same reason.
According to MLN Matters Article MM8863, the XE modifier can be used to indicate "A Service That Is Distinct Because It Occurred During A Separate Encounter." I've tried using the XE modifier to no avail.
Has anyone else had this same issue? Is it possible to get two payments when multiple encounters occur on the same date of service?