klmcginnis
New
- Messages
- 3
- Best answers
- 0
Hello,
We are experiencing denials from the Georgia CMO Medicaid plans when Z11.3 and Z30.09 are billed together. After following up, the plans provided the explanation below:
My question is:
Thank you,
Kim
We are experiencing denials from the Georgia CMO Medicaid plans when Z11.3 and Z30.09 are billed together. After following up, the plans provided the explanation below:
“The billed service (99211) was denied because the associated diagnosis codes, Z11.3 (Encounter for screening for infections with a predominantly sexual mode of transmission) and Z30.09 (Encounter for other general counseling and advice on contraception), should not be reported together.
Here is the CMS link showing excludes1 edits still apply for 2025:
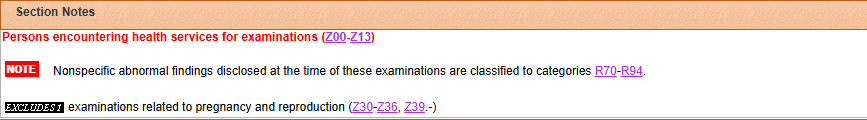
According to the ICD-10-CM Official Guidelines for Coding and Reporting: "An Excludes1 note indicates that the code excluded should never be used at the same time as the code above the Excludes1 note." This means the two conditions cannot occur together, such as a congenital form versus an acquired form of the same condition.
The code Z11.3 does have an Excludes 1 Note: Examinations related to pregnancy and reproduction (Z30-Z36, Z39.-), which means any code between Z30 and Z36. Since Z30.09 falls within this range, the edit fired as intended. For additional information, you may also reference Encoder and consult the ICD-10 manual for proper coding guidelines.”
This issue has only recently started occurring, despite the ICD reference they cite having been in the manual for several years.My question is:
- Is anyone else experiencing similar denials?
- Are there any known exceptions or guidance that supports billing these two codes together?
Thank you,
Kim