EricRmi
Contributor
Hi.
I need help getting paid when billing 90471, 90715 with patient-requested immunization, no counseling, Intramuscular, and only vaccine injected.
Patient went to the office requesting Tdap vaccination, as it has been more than 10 years since the last vaccination.
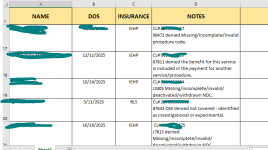
I get the same denial reason: "90471 denied for Missing/incomplete/invalid procedure code" every time.
I researched a lot due to this. The websites say the same sequence of coding; 90471 then 90715 which is what I am coding.
So please enlighten me. Thank you.
I need help getting paid when billing 90471, 90715 with patient-requested immunization, no counseling, Intramuscular, and only vaccine injected.
Patient went to the office requesting Tdap vaccination, as it has been more than 10 years since the last vaccination.
I get the same denial reason: "90471 denied for Missing/incomplete/invalid procedure code" every time.
I researched a lot due to this. The websites say the same sequence of coding; 90471 then 90715 which is what I am coding.
So please enlighten me. Thank you.