tmorgan808
Networker
- Messages
- 58
- Best answers
- 0
I have a question about infusion coding. The MAR has the following (I made the chart to make it easy to read):
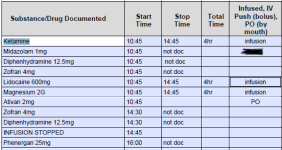
I am confused on how to code it. The initial would be the Ketamine 96365 x 1, 96366 x 3
There is not enough information in the chart note to indicate if the lido and mag were in a separate bag, same bag, not sure if I should allow concurrent.
Since there is not stop time for the other meds they would be considered IV push, but what about the ones with same start time as initial service?
Any help would be greatly appreciated.
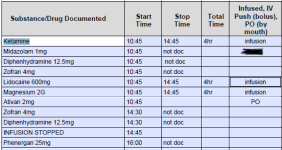
I am confused on how to code it. The initial would be the Ketamine 96365 x 1, 96366 x 3
There is not enough information in the chart note to indicate if the lido and mag were in a separate bag, same bag, not sure if I should allow concurrent.
Since there is not stop time for the other meds they would be considered IV push, but what about the ones with same start time as initial service?
Any help would be greatly appreciated.